What is the USAF target resolution test for 1951? - usaf target 1951
Eight of nine studies compared different techniques of refractive laser surgery. Two studies compared two different methods of flap procedures (i.e., LASIK versus SMILE).8,14 One study compared two different methods of surface procedures (i.e., LASEK versus PRK).15 One study compared a flap procedure with a surface procedure (i.e., LASIK versus PRK).11 One study compared a flap procedure (LASIK) with refractive lens exchange surgery using a femtosecond laser.12 Three studies compared a flap or a surface procedure of different platforms (i.e., symmetrical PresbyLASIK versus asymmetrical PresbyLASIK,16 tissuesaving PRK versus wavefront-optimized PRK,9 Wavefront-guided PRK versus Wavefront-optimized PRK10). One study compared LASIK with contact lenses, where patients switching from contact lenses to LASIK were compared with those who continued wearing contact lenses.13
The studies were conducted in the USA,10,13 the UK,12 Denmark,15 Singapore,8,14 Pakistan,11 Iran,9 and Spain,16 and were published in 2018,8 2017,11,12 2016,13 and 2015.9,10,14–16
The RCT by Sia et al., 201510 found no significant difference in patient satisfaction between wavefront-guided PRK versus wavefront-optimized PRK procedures.
Beamshaping
While care has been taken to ensure that the information prepared by CADTH in this document is accurate, complete, and up-to-date as at the applicable date the material was first published by CADTH, CADTH does not make any guarantees to that effect. CADTH does not guarantee and is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in any third-party materials used in preparing this document. The views and opinions of third parties published in this document do not necessarily state or reflect those of CADTH.
Liu, C.; Guo, Y. Flat-Top Line-Shaped Beam Shaping and System Design. Sensors 2022, 22, 4199. https://doi.org/10.3390/s22114199
The RCTs had an explicit research question, method of randomization, balance in patient characteristics between groups, and validated methods for outcome assessment. The nature of the study prohibited the blinding of staff and patients to condition assignment during treatment and follow-up periods that may have a risk of assessment bias. High follow-up rates were reported in two RCTs.8,10 Intention-to-treat analysis was not conducted in the RCTs. Overall, the RCTs were of moderate quality.
SuperGaussian
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
Except where otherwise noted, this work is distributed under the terms of a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International licence (CC BY-NC-ND), a copy of which is available at http://creativecommons.org/licenses/by-nc-nd/4.0/
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
The retrospective cohort study by Hashmani et al., 201711 found high and comparable in overall patient satisfaction rates between LASIK and PRK (93.3% versus 95.6%). Follow-up time was not specified.
Liu, C.; Guo, Y. Flat-Top Line-Shaped Beam Shaping and System Design. Sensors 2022, 22, 4199. https://doi.org/10.3390/s22114199
Liu C, Guo Y. Flat-Top Line-Shaped Beam Shaping and System Design. Sensors. 2022; 22(11):4199. https://doi.org/10.3390/s22114199
The retrospective cohort study by Schallhorn et al., 201712 found overall vision satisfaction (94.3% versus 79.1%; P < 0.01) and intention to recommend the procedure to a friend or a relative (98.9% versus 90.7%; P < 0.01) was significantly higher in LASIK compared to refractive lens exchange surgery in patients with moderate to higher myopia at the 3-month follow-up. However, no significant difference in patient satisfaction between groups for other refractive categories (i.e., low myopia, plano presbyopia, hyperopia).
CADTH is not responsible for any errors, omissions, injury, loss, or damage arising from or relating to the use (or misuse) of any information, statements, or conclusions contained in or implied by the contents of this document or any of the source materials.
ZIP-Document (ZIP, 159 KiB)
Laser beam
Abstract: In this study, the circular Gaussian spot emitted by a laser light source is shaped into a rectangular flat-top beam to improve the scanning efficiency of a selective laser sintering scanning system. A CO2 laser with a power of 200 W, wavelength of 10.6 μm, and spot diameter of 9 mm is shaped into a flat-top spot with a length and width of 0.5 × 0.1 mm, and the mapping function and flat-top Lorentzian function are calculated. We utilize ZEMAX to optimize the aspherical cylindrical lens of the shaping system and the cylindrical lens of the focusing system. We then calculate the energy uniformity of the flat-top line-shaped beam at distances from 500 to 535 mm and study the zoom displacement of the focusing lens system. The results indicated that the energy uniformity of the flat-top beam was greater than 80% at the distances considered, and the focusing system must precisely control the displacement of the cylindrical lens in the Y-direction to achieve precise zooming. Keywords: selective laser sintering; flat-top line beam; dynamic focus
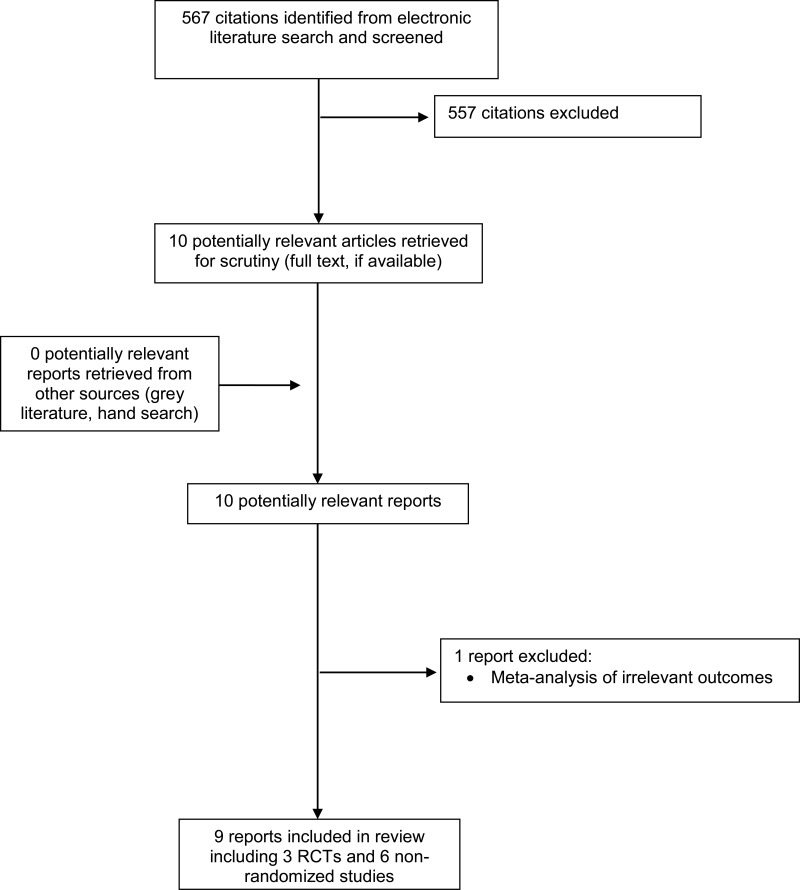
A total of 567 citations were identified in the literature search. Following screening of titles and abstracts, 557 citations were excluded and 10 potentially relevant reports from the electronic search were retrieved for full-text review. No potentially relevant publications were retrieved from the grey literature search. Of these potentially relevant articles, one publication was excluded due to irrelevant outcomes, while nine publications met the inclusion criteria and was included in this report. Appendix 1 presents the PRISMA flowchart of the study selection.
The SIGN checklists were used to assess the quality of the included RCTs6 and non-randomized studies.7 Summary scores were not calculated for the included study; rather, a review of the strengths and limitations were described narratively.
Refractive errors are vision defects caused by the change in shape of the cornea, a transparent surface that covers the eye ball, leading to improper focus of light rays on the retina.1,2 Laser refractive eye surgery refers to the use of laser techniques to correct refractive errors, such as myopia (nearsightedness), hyperopia (farsightedness) or astigmatism (uneven focusing).2,3 It uses excimer laser to reshape the cornea’s curvature to restore the refractive power of the eye, and ultimately to reduce or eliminate the need to wear glasses or contact lenses.1
The RCT by Damgaard et al., 20188 found no significant differences between LASIK and SMILE for all visual symptoms (light sensitivity, eye discomfort, eye dryness, excessive tearing, gritty sensation, glare, halos, blurring, fluctuations in vision) at the 3-month follow-up.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess.
This disclaimer and any questions or matters of any nature arising from or relating to the content or use (or misuse) of this document will be governed by and interpreted in accordance with the laws of the Province of Ontario and the laws of Canada applicable therein, and all proceedings shall be subject to the exclusive jurisdiction of the courts of the Province of Ontario, Canada.
Recent systematic review and meta-analysis found no significant differences in visual outcomes (efficacy and safety) or visual quality (post-operative higher-order aberrations and contrast sensitivity) among common used refractive surgical techniques, including LASIK, PRK, LASEK and Epi-LASIK.5 The visual outcomes were often accomplished in short-term studies, while long-term outcomes are still unclear.2 The aim of this report is to review the long-term clinical effectiveness of laser refractive surgery for vision correction in adults, with particular emphasis on the length of time to avoid corrective eye wear, patient satisfaction and quality of life. Cost-effectiveness of laser refractive surgery is also taken into consideration in this review.
The copyright and other intellectual property rights in this document are owned by CADTH and its licensors. These rights are protected by the Canadian Copyright Act and other national and international laws and agreements. Users are permitted to make copies of this document for non-commercial purposes only, provided it is not modified when reproduced and appropriate credit is given to CADTH and its licensors.
There are two main techniques of laser refractive eye surgery for vision correction:4 Flap or lamellar procedures: A thin flap of the corneal tissue is cut with either a microkeratome or a femtosecond laser and is lifted. A precise amount of tissue of the corneal stroma is removed with the microkeratome, an excimer laser or a specialized instrument, and then the flap is replaced. Three currently available procedures are Automated Lamellar Keratoplasty (ALK), Laser-Assisted in situ Keratomileusis (LASIK), and Refractive Lenticule Extraction (ReLEx), which is further subcategorized as Femtosecond Lenticule Extraction (FLEX) and Small Incision Lenticule Extraction (SMILE).Surface procedures: The most anterior tissue of the corneal stroma is ablated with an excimer laser without the need of a partial cut to create a corneal flap. Five different procedures are Photorefractive Keratectomy (PRK), Transepithelial photorefractive Keratectomy (TransPRK), Laser-Assisted Sub-Epithelial Keratomileusis (LASEK), Epithelial Laser Keratomileusis (Epi-LASIK), and customized Transepithelial No-touch (C-TEN).
Patients were adults with mean age ranging from 25 to 54 years with stable refraction. They underwent different types of laser refractive surgery to improve visual acuity and to seek independence from glasses or contact lenses. The refractive variables (e.g., sphere diopters [D], cylinder D, and spherical equivalent D) were comparable between groups, but varied across studies.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Subject to the aforementioned limitations, the views expressed herein are those of CADTH and do not necessarily represent the views of Canada’s federal, provincial, or territorial governments or any third party supplier of information.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
One prospective, longitudinal, parallel group, multicenter survey13 was identified that compared patient satisfaction among patients who continued wearing contact lenses with those elected to switch from contact lenses to refractive surgery using LASIK.
Studies were excluded if they did not satisfy the selection criteria in Table 1 and if they were published prior to 2013.
This review did not find any evidence on the long term clinical effectiveness of laser refractive eye surgery defined by the number of years that post-operative patients could stay independent from prescription glasses or contact lenses. Patient satisfaction and visual-related quality of life were identified as relevant outcomes in the included studies. One study compared LASIK with contact lenses, while the remaining eight studies compared different techniques of refractive laser surgery. Across studies, significant heterogeneity was noted for study designs, sample sizes, patient characteristics, surgery techniques, comparisons, patient satisfaction questionnaires, and follow-up periods. Seven out of nine studies were short-term with follow-up period ranging from 3 to 18 months, while one study had follow-up time of 3 years and the other had average follow-up time up to 6 years. Patient’s subjective experience, self-reported outcomes, and physician-related bias may have significant impacts in the study findings. All associated limitations (e.g., risk of selection and recalling bias, and confounders) of the non-randomized studies, particularly retrospective studies, would apply. No relevant literature could be identified for comparative cost-effectiveness of laser refractive surgery with other laser techniques or with other methods of vision correction.
The longitudinal, comparative case series by Soler Tomas et al., 201516 reported comparative results of patient satisfaction between symmetrical and asymmetrical presbyLASIK after 18 months. The study found no significant difference in patient satisfaction between the two procedures.
This document is prepared and intended for use in the context of the Canadian health care system. The use of this document outside of Canada is done so at the user’s own risk.
The summary of the quality assessment for the RCTs and observational studies was described below and is presented in Appendix 3.
Liu, Che, and Yanling Guo. 2022. "Flat-Top Line-Shaped Beam Shaping and System Design" Sensors 22, no. 11: 4199. https://doi.org/10.3390/s22114199
Liu, Che, and Yanling Guo. 2022. "Flat-Top Line-Shaped Beam Shaping and System Design" Sensors 22, no. 11: 4199. https://doi.org/10.3390/s22114199
A limited literature search was conducted on key resources including PubMed, The Cochrane Library, University of York Centre for Reviews and Dissemination (CRD), Canadian and major international health technology agencies, as well as a focused Internet search. Methodological filters were applied to limit retrieval to systematic reviews, meta-analyses, health technology assessments, randomized controlled trials, non-randomized studies, and economic studies. Where possible, retrieval was limited to the human population. The search was also limited to English language documents published between January 1, 2013 and May 27, 2018.
This document may contain links to third-party websites. CADTH does not have control over the content of such sites. Use of third-party sites is governed by the third-party website owners’ own terms and conditions set out for such sites. CADTH does not make any guarantee with respect to any information contained on such third-party sites and CADTH is not responsible for any injury, loss, or damage suffered as a result of using such third-party sites. CADTH has no responsibility for the collection, use, and disclosure of personal information by third-party sites.
Liu C, Guo Y. Flat-Top Line-Shaped Beam Shaping and System Design. Sensors. 2022; 22(11):4199. https://doi.org/10.3390/s22114199
All three RCTs recruited patients from a single centre. Two RCTs9,10 were open-label, two arms, parallel, and had a 1:1 ratio. One RCT8 was prospective, paired-eye, single-masked study, in which each patient was randomized to undergo one procedure in one eye and other procedure in the other eye (performed by the same surgeon) on the same day.
The identified outcomes from the included studies were patient satisfaction8–13,15,16 and visual-related quality of life14 using validated questionnaires. Other outcomes such as length of time to maintain clinical effectiveness (defined by number of years patients avoid the need for eye glasses or contact lenses) and the need for corrective eye wear were not identified.
All non-randomized studies addressed an appropriate and clearly focused question, had balance patients characteristics between groups, and used reliable and validated methods of assessment. All studies had high risk of selection bias as the participant rate was not defined in the prospective cohort studies,13,14 or it was not applicable in the retrospective cohort studies.11,12,15 The rate of follow-up between groups was not reported in the prospective cohort studies13,14 or in the longitudinal comparative case series16 that may result in the risk of attrition bias. Blinding was not possible in retrospective cohort studies and many prospective cohort studies that may have a risk of detection bias. All studies did not identify and control for potential confounding variables in their analyses. Overall, the included observational studies were at high risk for bias.
D = diopters; ITT = intention-to-treat; LASEK = laser-assisted subepithelial keratectomy; LASIK = laser in-situ keratomileusis; NR = not reported; PP = per protocol; PRK = photorefractive keratectomy; QIRC = Quality of Life Impact of Refractive Correction; QoL = quality of life; RCT = randomized controlled trial; RLE = refractive lens exchange; SD = standard deviation; SMILE = small incision lenticule extraction
The RCT by Nassiri et al., 20159 found no significant difference in patient satisfaction between tissue-saving PRK and wavefront-optimized PRK procedures.
The retrospective cohort study by Hansen et al., 201515 found high patient satisfaction rates in both LASEK and PRK groups with no significant difference (92% versus 100%; P = 0.87) at an average follow-up time of 6.0 years and 4.6 years, respectively.
Evidence on long-term clinical effectiveness of laser refractive surgery for vision correction defined as the number of years that a patient remains independent of corrective eyewear was not identified. Patients who underwent Laser-Assisted in situ Keratomileusis reported having higher overall patient satisfaction compared to those wearing contact lenses. No difference in patient satisfaction or vision-related quality of life was detected among refractive eye surgery techniques. No relevant literature on the cost-effectiveness of laser refractive eye surgery was identified.
Ten questions on patient perception of glare, light sensitivity, hazy or foggy vision, dry eye, foreign body sensation, vision fluctuation, double vision.
Data analysis in two RCTs was performed using per protocol approach.8,10 Sample size calculation was applied in two RCTs8,9 and one cohort study.14 The remaining studies did not report on methods of analysis or sample size calculation. Instead, only P value set at 0.05 or 0.01 was used for the comparison between interventions.
One reviewer screened citations and selected studies. In the first level of screening, titles and abstracts were reviewed and potentially relevant articles were retrieved and assessed for inclusion. The final selection of full-text articles was based on the inclusion criteria presented in Table 1.
Of the six non-randomized studies, three were retrospective cohort studies,11,12,15 two were prospective cohort studies,13,14 and one was comparative case series.16
The characteristics of the identified studies including three RCTs8–10 and six nonrandomized studies11–16 are summarized below and are presented in Appendix 2.
Laser refractive surgery for vision correction. Ottawa: CADTH; 2018 June. (CADTH rapid response report: summary with critical appraisal).
Overall satisfaction (i.e., strongly agree that they would recommend their current method to a friend or a family member) was higher in LASIK after contact lens group (88%, 84%, 88%) than contact lens control groups (60%, 61%, 54%) at 1-, 2-, and 3-year surveys, respectively. The proportion of patients who reported no difficulty with night-driving and night visual disturbances were also higher in LASIK group compared to contact lens group. The frequencies of other outcomes such as dry eye, difficulty reading small print, depression, eye infection, eye ulcer and eye abrasion did not change from baseline to follow-up surveys and were comparable between groups.
Disclaimer: The information in this document is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. While patients and others may access this document, the document is made available for informational purposes only and no representations or warranties are made with respect to its fitness for any particular purpose. The information in this document should not be used as a substitute for professional medical advice or as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process. The Canadian Agency for Drugs and Technologies in Health (CADTH) does not endorse any information, drugs, therapies, treatments, products, processes, or services.
A laser refractive surgery for vision correction such as LASIK technology was found to yield higher levels of patient satisfaction compared to contact lens wear. There was no significant difference in subjective visual symptoms, patient satisfaction, or visual-related quality of life between different laser refractive surgery techniques, or between different platforms of a laser refractive surgery technique. Due to short-term follow-up and limited number of studies identified for each type of comparison (often single study), it is still uncertain about the reproducibility of the findings, thus the interpretation should be taken with caution. The current literature regarding laser refractive eye surgery primarily emphasizes visual and refractive outcomes, and showed no significant differences among most surgical techniques. Studies that aim to determine the number of years for which laser refractive eye surgery for vision correction could keep patients from returning to prescription glasses or contact lens wear would reduce uncertainty. Additionally, as no cost-effectiveness studies were identified, high quality studies examining the comparative cost-effectiveness of the various surgery techniques are needed in order to determine cost-effectiveness.
The prospective cohort study by Ang et al., 201514 found no significant difference in visual-related quality life (assessed using Quality of Life Impact of Refractive Correction questionnaire) between LASIK and SMILE at the 1- and 3-month follow-ups.
D = diopters; ITT = intention-to-treat; LASEK = laser-assisted subepithelial keratectomy; LASIK = laser in-situ keratomileusis; NR = not reported; PP = per protocol; PRK = photorefractive keratectomy; QIRC = Quality of Life Impact of Refractive Correction; QoL = quality of life; RCT = randomized controlled trial; RLE = refractive lens exchange; SD = standard deviation; SMILE = small incision lenticule extraction; UCVA = uncorrected visual acuity; VRQoL = vision-related quality of life




 Ms.Cici
Ms.Cici 
 8618319014500
8618319014500