Waveplates - Prisms & Polarizers - Optics - quarter waveplate
Tendons and ligaments
Interestingly, another Chinese study found that, while SMILE is as effective as FS-LASIK in correcting high myopia, attention should be paid to the induction of vertical coma in highly myopic patients following SMILE.3
According to Dr. Manche, one of the advantages of LASIK is that it’s been around a long time, with tens of millions of procedures having been performed. “It’s a very well-known and mature technology,” he says. “SMILE was approved in the United States in 2016, and about 3 million cases have been performed worldwide.”
Tendons are unique connective tissues that not only connect the muscles and bones, but they are also important for maintaining posture and locomotion through transmitting muscle-contraction force to the skeleton. The tendon is composed predominantly of tenocytes surrounded by extracellular matrices (ECM) such as collagen I fibers, proteoglycans, and glycoproteins. It forms a solid structure and can support high repetitive mechanical loading (1). However, tendon tissue has poor healing ability and limited regenerative ability; the damage may become irreversible, and the healing process will be difficult, leading to chronic disability. Although the current wide use of topical or systemic anti-inflammatory drugs can reduce the perception of pain, and surgical repair of ruptured tendons through autograft or allograft seems to maintain the physiological function of the tendon (2), the functional, structural, and biochemical properties of the damaged tendon cannot be fully restored to an uninjured status (3). In addition, the repair process may induce the formation of scar tissue (4), of which the tensile strength is only one-third that of an undamaged tendon, which can be a triggering factor for a large number of cases of secondary damage (5). Furthermore, autograft may cause donor site morbidity, while allograft may elicit an immune rejection (6).
Another available cell type is pluripotent stem cells, which can differentiate into all types of cells constituting the human body. These include embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), which can be derived from differentiated human dermal fibroblasts (21).
Find many great new & used options and get the best deals for Diffraction Grating Film - Window Suncatcher and Rainbow Maker Film at the best online prices ...
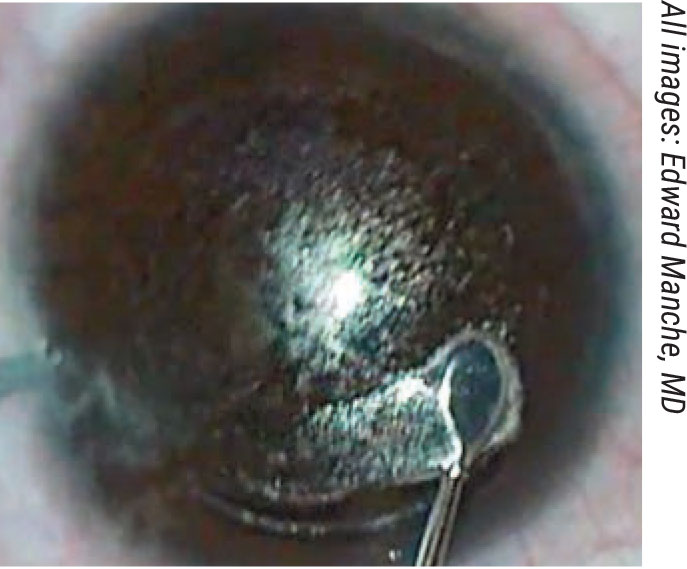
Additionally, studies have shown that, compared to LASIK, SMILE provides potentially better biomechanical stability of the cornea. “Some very good work has shown that the anterior lamellar tissue in the cornea is the strongest,” Dr. Manche says. “SMILE spares the anterior corneal lamellar tissue. The side incision with SMILE is only 4 mm compared to the 20-mm incision with LASIK. There’s significantly more transection of the corneal lamellae with LASIK compared to SMILE. Preservation of the anterior stromal tissue results in a reduced biomechanical insult to the cornea with SMILE, and that could have implications with regard to lowering the risk of ectasia.”
Ligament
Abstract: There is a high risk of injury from damage to the force-bearing tissue of the tendon. Due to its poor self-healing ability, clinical interventions for tendon injuries are limited and yield unsatisfying results. Tissue engineering might supply an alternative to this obstacle. As one of the key elements of tissue engineering, various cell sources have been used for tendon engineering, but there is no consensue concerning a single optimal source. In this review, we summarized the development of tendon tissue from the embryonic stage and categorized the used cell sources in tendon engineering. By comparing various cell sources as the candidates for tendon regeneration, each cell type was found to have its advantages and limitations; therefore, it is difficult to define the best cell source for tendon engineering. The microenvironment cells located is also crucial for cell growth and differentiation; so, the optimal cells are unlikely to be the same for each patient. In the future, the clinical application of tendon engineering might be more precise and customized in contrast to the current use of a standardized/generic one-size-fits-all procedure. The best cell source for tendon engineering will require a case-based assessment.
The 160mm standard objectives are interchangable among each other, but not with infinity. In short, you can not connect an objective with a ...
Tendons are an important component in the musculoskeletal system. Due to the limited regenerative ability of tendons, the healing process after an injury is slow, and the functions of the tendon are likely to be compromised. This results in a serious decline in the quality of life of patients. Cell-based tendon tissue engineering is a promising research area that aims to deliver adequate, regeneration-competent cells to the injured tendon and ultimately promote the restoration of its functions (20). This review provides an overview of tendon tissues from an embryonic stage and discusses the relative merits of each of the candidates that could be used as cell sources for tendon regeneration. Depending on the characteristics of each cell type, the researchers tested the most appropriate mechanical stimulation conditions and selected the different biological factors for improving the healing quality of the damaged tendon and reducing the adverse reactions during use (Table 5). Some major findings are described below: Mechanical stimulation will enhance the tenocyte differentiation in different cell types. Growth factors can promote cell proliferation in differentiated cells. However, in stem cells, growth factors not only enhance tenogenic differentiation but also increase the rate of cell growth. Furthermore, cell ECM also can accelerate cell proliferation and the tenogenesis of MSCs. Therefore, the results of these studies may provide new concepts or methods in clinical treatment to improve the level of tendon repair in patients. Doctors can select different cells to treat tendon disease by measuring a patient’s expression level of growth factors, tendon transcription factors, the expression of collagen and cytoskeletal proteins in the extracellular matrix, and the microenvironment of the tendon. Clinical treatment of tendon injury can also provide an appropriate cell plan by avoiding the drawbacks of these seed cells. Massive ectopic ossification and fatty vesicles forming in the tendinopathy indicate that BMSCs and ADSCs are not the best choices in the treatment of tendinopathy (115). In addition, scar formation and disorganization of fibers at tendon damage or stump are factors to be considered when selecting candidate cells.
The role of the Helium gas in He-Ne laser is to increase the efficiency of the lasing process. Two effects make Helium particularly valuable:.
1Department of Orthopedics, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, School of Medicine, South China University of Technology, Guangzhou Higher Education Mega Centre, Guangzhou 510006, China;2Centre for Orthopaedic Translational Research, School of Biomedical Sciences, University of Western Australia, Nedlands, Western Australia, Australia
Dermal fibroblasts are terminally differentiated cells that originate from mesoderm. In vitro, dermal fibroblasts exhibit similar cell morphology as tenocytes and mainly produce col I and col III. Compared with tenocytes, the harvest of dermal fibroblasts is less defective as only an easily accessible, small piece of skin is needed. Also, the cell expansion is less likely during in vitro culture (31). It has been revealed that there is no difference in their gross view between neo-tendon tissues engineered by human dermal fibroblast or tenocytes. There was also no difference found in the histologic structure, collagen superstructure, or mechanical property under the static strain in vitro (32-34). Therefore, researchers have used dermal fibroblast-engineered tendon to repair animal tendon defect, and the results are satisfactory in that the tensile stiffness and maximum load are expressly higher than those of non-dermal fibroblast scaffolds (35-38).
1. Aygun BT, Cankaya KI, Agca A, et al. Five-year outcomes of small-incision lenticule extraction vs femtosecond laser-assisted laser in situ keratomileusis: A contralateral eye study. J Cataract Refract Surg 2020;46:3:403-409.
As mentioned above, outcomes of the two procedures are quite comparable. Dr. Manche just completed a randomized clinical trial of 40 patients who underwent wavefront-guided LASIK in one eye and SMILE in the fellow eye. He assessed patients at one, three, six and 12 months. “We did find slightly better outcomes with wavefront-guided LASIK compared to the SMILE surgery,” he says. “We had slightly more LASIK eyes achieve an uncorrected visual acuity of 20/20, as well as higher levels of visual acuity of 20/16 and 20/12.5. Additionally, we had greater gains of lines of best-corrected visual acuity in the wavefront-guided LASIK group compared to the SMILE group. So, on the whole, the outcomes were very similar, but there were small but measurable benefits to wavefront-guided LASIK compared to SMILE.” Dr. Manche will be presenting the results of this study at this year’s meeting of the American Society of Cataract and Refractive Surgery.
John Vukich, MD, who is in practice in Wauwatosa, Wisconsin, was one of the primary investigators for SMILE and VisuMax and has a long history of performing LASIK. “In my previous refractive surgery practice, we were considering SMILE to be a premium procedure, so we were charging slightly more for it,” he says. “We believe that SMILE and LASIK aren’t completely equivalent and, physiologically, SMILE may have some advantage over LASIK, the more traditional option. SMILE is the newer technology, has a very good safety profile, and preserves a greater amount of integrity of the structure of the cornea.”
In the process of tendon development, tenocytes are the terminal product and the major component of the tendon’s structure. Dermal fibroblasts belong to the class of mesenchymal cells, which are differentiated from MSCs. As dermal fibroblasts are labile cells and have the same precursors as tenocytes, they can be used in tendon repair (17).
The objective is the most difficult component of an optical microscope to design and manufacture, and is the first component that light encounters as it ...
Aims and ScopeAnnals of Translational Medicine (Ann Transl Med; ATM; Print ISSN 2305-5839; Online ISSN 2305-5847) is an international, peer-reviewed, open access journal, aiming to provide multidiscip...
Additionally, LASIK has faster visual recovery. “When SMILE was initially approved in the United States, we were using relatively high energy levels,” Dr. Manche says. “ The use of higher energy levels in SMILE surgery has been associated with significantly slower visual recovery. So, when SMILE was first released, many patients experienced slower recovery of vision. It was common to have patients seeing 20/40 or 20/30 on postoperative day one. This is in contrast to what you see with LASIK, after which the majority of patients see 20/20 or 20/15 on day one.”
LASIK has been performed for more than 30 years with impressive results, but surgeons and patients are always on the lookout for something new and—possibly—improved. It’s with this mindset that eyes were turned toward the relative newcomer in the refractive surgery marketplace, small-incision lenticule extraction, performed with the VisuMax femtosecond laser (Carl Zeiss Meditec; Jena, Germany). Even though SMILE is in its relative infancy as a go-to refractive procedure, it’s producing results similar to advanced LASIK—but it’s not without its issues. Here, experts discuss the relative merits of the two procedures, and we also look at the results of well-performed studies of the surgeries.
Cells found in tendons are called
Dr. Vukich says he’s encountered patients who have done research and have come to the conclusion that SMILE was a better procedure for them. “You try to be even-handed,” he says. “The majority of our cases remained LASIK, however. When given the choice, some of the decision was driven by the price differential, some of it was driven by familiarity and some of it was driven by just the potential longevity of exposure to LASIK.
Therefore, tissue engineering has been explored in an attempt to improve tendon healing and eventually reach a complete biological repair. A classic tissue engineering (7) technique is to culture seed cells in an engineered structure that is made of a biodegradable scaffold with the supplementation of growth factors or either mechanical or chemical factors to promote cell proliferation and differentiation in vitro before it is transplanted into the damaged site in vivo. Subsequently, the scaffold could be substituted by a newly formed organization that can replace damaged tissues and ultimately reconstitute the tissue functions (8). In tendon tissue engineering, cells also play a vital role in producing ECM for the reconstruction of the tendon tissue structure (9). Thus, the source of the seed cells becomes one of the key points in tendon tissue engineering. To find more potential candidates suitable for tendon tissue engineering, we explore the embryological origin of the limb tendons, analyze the developing processes of tendons, and summarize the availability of various types of seed cells using tendon tissue engineering. So, at the beginning of the article, we will reconstruct the development of the tendon from the embryo to maturity and explain the availability of these cells.
The use of ESCs may be limited due to the need to sacrifice an embryo, which has aroused some ethical controversy. The discovery of iPSCs resolves the ethical problem of using ESCs, and recently, researchers were able to generate iPSCs from terminally differentiated cells (21,61). However, as their iPSCs were generated using retroviruses or lentiviruses (62), it might cause mutagenesis that would pose a risk for adverse effects in therapy (63). The efficiency of the transfection process also remains low. Thus, for the purpose of the safety of cell transplantation therapy, mRNA-delivered transcription factors have been applied to generate integration-free iPSCs (64,65). While these studies address some of the issues raised by the use of iPSCs in regenerative medicine, it has not been reported in tendon tissue engineering. For now, iPSCs are being used as a potential seed cell source for tendon regeneration research.
Tendon cellfunction
When dermal fibroblasts and tenocytes are compared, both originate from mesoderm and have similar morphologies (36), and it was determined that dermal fibroblasts were more advantageous compared to tenocytes. First, dermal fibroblasts have good proliferative capacity and self-renewal potential (39). Second, dermal fibroblasts have been shown to be easy to harvest with no major tissue defects at the donor site since the skin can regenerate in a short time (40). In contrast, tenocytes are more difficult to collect because the density of tenocytes in a tendon is low, and there is an issue of donor site morbidity (41). However, dermal fibroblasts have a disadvantage in that they may produce fibrotic ECM which is involved in scar formation (42) (Table 2).
For another perspective, a recent study conducted in China found that, when compared to LASIK, SMILE may offer better safety and objective visual quality, comparable stability and efficacy, but slightly inferior predictability when correcting myopia exceeding 10 D.2 This prospective, randomized, comparative study included 60 eyes in 60 patients. Thirty eyes were corrected using SMILE, and 30 were corrected using FS-LASIK. Patients received preoperative and six-month postoperative examinations.
Tendonstructure
Iris Diaphragms ... Motorized iris diaphragms are used in the fields of optoelectronics, lasers and medical technology, among others. They allow optical setups to ...
Based on the process of limb tendon development, tenocytes originate from mesenchymal stromal cells (MSCs), which are also progenitor cells of skeletal elements and other connective tissues. Limb bud MSCs are derived from the lateral plate mesoderm of the embryo. These cells at different stages of tendon differentiation are candidate types of seed cells in tendon tissue engineering.
Postoperative spherical equivalent refraction was -0.20 ±0.25 D in the SMILE eyes and -0.03 ± 0.20 D in the LASIK eyes, and the posterior corneal curvature was unchanged after both procedures. The measured corneal thickness was reduced by 137.40 ±15.01 µm in the SMILE eyes and by 155.06 ±17.43 µm in the LASIK eyes. The change in the SE was -0.01 ±0.26 D in the SMILE eyes and -0.13 ± 0.30 D in the LASIK eyes after one week. Only the peak distance (the distance between the highest points of the nondeformed corneal parts) differed between the groups; the distance was 1.06 ±1.44 mm in the SMILE eyes and -0.26 ±1.16 mm in the LASIK eyes. The SMILE eyes had smaller changes in higher-order aberrations and spherical aberration than the LASIK eyes.
This prospective, comparative study included 52 eyes of 34 consecutive highly myopic patients with spherical equivalent between -8 and -10 D. Twenty-three eyes of 16 patients underwent FS-LASIK, while 29 eyes of 18 patients underwent SMILE. Visual outcomes and wavefront aberrations were analyzed preoperatively and six months postoperatively.
Tenocytes are highly specialized mesenchyme-derived cells with important roles in synthesizing ECM and maintaining tendon structures in vivo (23). Cao et al. constructed tissue-engineered artificial tendons for the first time (24), but they also indicated that tenocytes are relatively difficult to grow and expand in vitro. Furthermore, some researchers indicated that with increased passaging, the gene expression of tendon-associated proteins such as collagen type I (col I), collagen type III (col III), tenascin, and tenomodulin (TNMD) exhibited a trend of decrease (25). In addition, there is also a change in the tenocyte cell phenotype, represented by more rounded cell morphologies instead of longer and thicker configurations (18). Thus, many researchers have explored the strategies to promote proliferation and at the same time, support a stable phenotype of tenocytes. At present, it has been reported that thyroid hormone T3, transforming growth factor (TGF)-b1, glycine, platelet-rich plasma, and insulin-like growth factor 1 could enhance the proliferation and differentiation capacity of tenocytes, as well as stimulate the secretion of ECM (23,26-29). Mechanical force can also regulate tenocyte differentiation (30).
Tendon cellinflammation
Pertinent to the article’s topic, Dr. Manche performs sponsored research for Alcon, Carl Zeiss Meditec and Johnson & Johnson Vision. He is a consultant for Johnson & Johnson Vision. Dr. Vukich has no financial interest in any of the products discussed.
2. Yang X, Liu Q, Liu F, Xu J, Xie Y. Comparison of outcome between small incision lenticule extraction and FS-LASIK in eyes having refractive error greater than negative 10 diopters. J Cataract Refract Surg 2020;46:1:63-71.
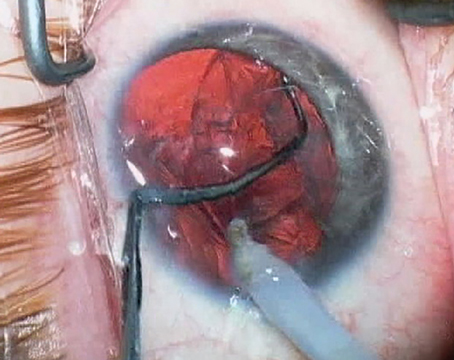
Another advantage of LASIK is that it’s easy to do a touch-up. Surgeons can lift the flap and perform a retreatment. “In comparison, surgeons cannot perform a repeat SMILE surgery on an eye that’s already had SMILE,” notes Dr. Manche. “If an eye that has previously had SMILE requires an enhancement procedure, you are left with a couple of options. You can perform LASIK surgery by cutting a flap in the SMILE cap. In the United States, the SMILE cap thickness is defaulted at 120 µm, so you then have to cut a LASIK flap at either 90 µm or 95 µm, which only gives you about 25 to 30 µm of play between the cap cut and the flap cut. Some surgeons aren’t comfortable with that. Another choice is to perform a side cut and open up the original 120-µm SMILE cap and convert that into a LASIK flap. A final choice is to perform PRK surgery on top of the SMILE cap. I don’t like to cut a LASIK flap 25 to 30 µm away from the SMILE cap interface, so I perform PRK touch-ups for all of my SMILE enhancements.”
May 1, 2014 — High strength optically clear glass bonding UV-cure adhesive is ideal for bonding architectural glass and furniture.
Magnifying Glass · Magnifying Glass · Sign Up for Email & Save 10% · Thank you for signing up. · Missing Fields · Find a Class Code. 1 ...
Since there is such a large variety of individual complexity for each of the patients undergoing clinical treatment, it is difficult to define optimal cell sources in tendon engineering. There are various types of tendon damage, including tendon rupture, tear, degeneration, tendinopathy, etc., which might change the cellular status at the damage site (116), and eventually affect the treatment outcomes. Furthermore, stem cell quality varies widely for different individuals. Therefore, there is no best cell source for tendon engineering in general. The determination of the most suitable cell source should be based on a comprehensive assessment of each patient. In the future, clinical treatment of tendon injury by tissue engineering should be customized designed on a case-by-case basis to achieve the best clinical outcomes.
Funding: This study was supported by the National Natural Science Foundation of China (81802214;81702191; 81371991), the National Natural Science Foundation of China Youth Science Foundation (81802222), the Major Program of Science and Technology of Guangdong (2015B020225007), the Natural Science Foundation of Guangdong Province (2018A030310694), the Fundamental Research Funds for the Central Universities, South China University of Technology (2018MS70), and the Guangdong Medical Science and Technology Research Foundation (2018114214430383). The Fundation of Traditional Chinese Medicine of Guangdong Province (20191004), The scientific Foundation of Guangdong Provincial People’s Hospital (2017bp01), The Outstanding Young Talents Foundation of Guangdong Provincial People’s Hospital (KJ012019091), Prrogam of Science and Technology of Guangzhou (201904010424).
The Elcometer 7062 MarSurf PS10 Surface Roughness Tester is a light and portable gauge used to measure surface roughness in accordance with International ...
TDSCs isolated from human tendons have general stem cell characteristics such as clonogenicity, multipotency, and self-renewal capacity (95,96). TDSCs can spontaneously regenerate tendon-like tissue structures in vivo and avoid differentiating into other kinds of cell lines. Extensive progress and deep insights have emerged in the study of these cells for tendon tissue engineering and regeneration (19). ECM (97), biglycan (98), hepatocyte growth factor (99), and mechanical stimulation (100) that can promote TDSCs proliferation and tenogenic differentiation in vitro have been verified in research. CTGF and ascorbic acid can enhance the survival time, proliferation, and migration abilities of TDSCs in vivo (101). Recently, Zhang et al. demonstrated that genetic alterations of TDSCs following culture expansion could be prevented by pretreating TDSCs with histone deacetylase inhibitor, to retain their ability to accelerate tendon repair in vivo (102). Furthermore, Yin et al. identify a subpopulation of nestin+ TDSCs which exhibited a superior tenogenic capacity compared with nestin- counterparts (103). This study not only redefines the subpopulation of tendon stem cells but also provides new insights into a novel cell line for tendon tissue engineering.
All content on this site: Copyright © 2024 AME Publishing Company. All rights are reserved. For all open access content, the Creative Commons licensing terms apply.
Tendonfunction
At six months postoperatively, the uncorrected distance visual acuity was -0.01 ±0.06 logMAR (a little better than 20/20) in the SMILE eyes and -0.05 ± 0.10 (a little better still) in the LASIK eyes, while the corrected visual acuity was -0.07 ± 0.07 logMAR in the SMILE eyes and -0.08 ± 0.08 (a shade off of 20/16) in the LASIK eyes.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
At the six-month visit, 96.6 percent of eyes in the SMILE group and 91.3 percent in the FS-LASIK group achieved unchanged or better best-corrected distance visual acuity. Additionally, 96.6 percent of eyes in the SMILE group and 95.7 percent in the FS-LASIK group achieved uncorrected distance visual acuity of 20/20 or better. As for wavefront aberrations, high-order aberrations and spherical aberrations increased significantly after surgery in both groups relative to preoperative values, and vertical coma increased after SMILE. Other than the difference in vertical coma, there were no statistically significant differences in the changes in higher-order aberrations, spherical aberrations, horizontal coma, coma, horizontal trefoil, vertical trefoil or trefoil between the two groups.
3. Yang W, Liu S, Li M, Shen Y, Zhou X. Visual outcomes after small incision lenticule extraction and femtosecond laser-assisted LASIK for high myopia. Ophthamic Res 2020;63:4:427-433.
In summary, the available seed cells for tendon tissue engineering include ESCs, iPSCs, MSCs (included BMSCs, ADSCs, and TDSCs), dermal fibroblasts, and tenocytes, as summarized in Figure 2. Next, we will discuss the respective advantages and disadvantages of these different cell types.
According to Dr. Vukich, SMILE is another step in the evolution of corneal recontouring as it relates to a refractive outcome. “We have data to support that the intrastromal removal of tissue versus the creation of a cap leaves intact a greater percentage of the corneal strength and integrity, and we believe that to be an advantage in the long run,” he says. “Many patients seeking refractive surgery are in their 20s and 30s, and they’re making decisions with the understanding that they will need to have healthy eyes and good vision for maybe another 70 years. All things being equal, a greater percentage of retained corneal structural integrity is a tiebreaker for many people.”
Fallout Laser Musket Rifle Replica 1:1 Fan Art prop ... Fallout 4 Laser Pistol Splitter ...
Edward Manche, MD, director of the Cornea and Refractive Surgery Service at Stanford University School of Medicine, has been performing SMILE surgery since it was approved in 2016, so he’s familiar with the trade-offs of each. “Both LASIK and SMILE work very well,” he says. “Both provide excellent outcomes and safety, and both can be used in about 85 percent of all patients that come into a typical practice. However, SMILE isn’t yet approved for hyperopia or mixed astigmatism. In addition, in the United States, we’re limited to 3 D of astigmatism or less with SMILE. So, within those parameters, SMILE and LASIK have a pretty wide approval, and a lot of the choice in procedure comes down to patient preference.”
The BMSCs have active self-proliferative and multi-differentiate capacity. The use of autologous BMSCs in the animal model could induce matrix production and organization of injured tendon as well as restore histological structure and function (71). Because of the easy isolation from bone marrow and the enrichment of colony-forming units, BMSCs have become an attractive cell source for tissue engineering approaches. However, BMSCs may differentiate into osteoblasts instead of the expected tenocyte lineage when transplanted into the injured tendon, and form ectopic bone in vivo (72,73). To overcome such issue, a number of approaches are presently being developed to navigate the tenogenic differentiation of BMSCs (74). They have shown that cyclical uniaxial stretching and BMP14, TGF-β, connective tissue growth factor (CTGF), vascular endothelial growth factor (VEGF), and myostatin can initiate and maintain highly efficient growth and differentiation of BMSCs towards tenocytes in vitro (75-80). Furthermore, Zhang et al. (78) and Xie et al. (81) used a 3D culture environment combined with BMSCs sheets that have therapeutic effects on improving the healing quality of the tendon in vivo.
“The quality of vision is very high for both procedures,” he adds. “Sometimes, there’s a day or two of additional recovery time for SMILE. However, there’s also always the possibility of delayed healing with LASIK, whether it be from striae or epithelial issues related to drops or other things. So, I would say the procedures are roughly equivalent in terms of acuity and patient satisfaction.”
According to the differentiation potential, stem cells can be divided into distinct kinds of cell types. Pluripotent stem cells can differentiate into all cell types of all organs, like ESCs and iPSCs (43). Multipotent stem cells can develop into many cell types within a particular lineage. For instance, the MSCs can give rise to bone cells, cartilage cells, adipose cells, and tendon cells. As ESCs have unlimited self-renewal potential and can differentiate into cells of all three embryonic germ layers (44), the risk of developing teratoma is expected to increase (45).
SMILE was first approved in the United States for spherical myopia. A second approval for the treatment of compound myopic astigmatism came in 2018. With the second approval, surgeons were finally allowed to make adjustments to the energy levels. “The Zeiss clinical care specialist, in concert with the surgeon, carefully adjusts the energy levels to the point where the surgeon can still achieve easy lenticule dissection, but where they’re not seeing much of the opaque bubble layer,” explains Dr. Manche. “Lower energy levels can provide significantly better uncorrected visual acuity from postop day one. With the lower energy settings, we’re now seeing patients who are 20/20 or 20/25 on day one. We even see an occasional patient at 20/15 or better. The postoperative day one vision is still not quite as good as with LASIK, but it’s significantly better than what we saw in the early approval with our standard, fixed, higher treatment energy levels.”
MSCs are non-hematopoietic adult stem cells derived from the mesoderm germinal layer that can differentiate into mesenchymal-derived cell types and have the ability to self-renew (66). The membrane surface of MSCs expresses several antibodies, such as stromal cell antigen-1, CD271, stage-specific embryonic antigen-4, CD146, and so on, which can be considered as specific markers of MSCs (67,68). MSCs were initially isolated from bone marrow as precursors of stromal elements (69). From recent research, it is now clear that MSCs can be isolated from a wide range of adult and perinatal mesenchymal tissues, including those of bone, synovial membranes, periosteum, adipose tissue, tendons, skeletal muscles, and others (70). The use of MSCs for tendon repair has been extensively explored and may promote tendon regeneration.
Tendon cellstructure
By contrast, MSCs are more safe due to their limited proliferation capacity and the restricted multilineage differentiation potential of cells of the mesodermal lineage (48,49). The use of MSCs also bypasses certain ethical obstacles as they are adult stem cells that can be harvested from non-embryonic sources (50). However, it has been accepted that MSC expansion in culture results in their accelerated aging, which will cause the deficiency of proliferation and multilineage differentiation potential (51,52) (Table 3).

Contributions: (I) Conception and design: F Qi, T Wang, Q Zheng; (II) Administrative support: None; (III) Provision of study materials or patients: Z Deng; (IV) Collection and assembly of data: F Qi; (V) Data analysis and interpretation: F Qi; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.
MSCs can be harvested from various sources, such as bone marrow, adipose fat, and tendon tissue. They have paracrine effects, including immunomodulation, promoting angiogenesis, or suppressing inflammation and immune cell functions through secretory factors (106). BMSCs were the first discovered MSCs and the most widely used seed cells in tissue engineering. They are easy to harvest through bone marrow aspiration, but their limitations include relatively small quantities of viable cell yield through an invasive method, which cause many complications on the donor site and ectopic ossification after transplantation in vivo (107,108). ADSCs can be obtained from liposuction aspirates, which is less invasive and involves lower risk. With the relatively large storage of adipose tissue in vivo, a mass of ADSCs can be isolated and expanded in vitro (109,110). However, the main disadvantage of ADSCs is their tendency to undergo adipogenesis in vivo (111). TDSCs express higher tendon-related markers and differentiation factors than BMSCs and ADSCs (112,113), but the main drawback of TDSCs is that their isolation will lead to the injury of the donor site (114). Overall, there is not enough data from practical research on TDSCs to make firm or extensive conclusions (Table 4).
Meanwhile, considering that ESCs originate from the blastocyst, the harvest of human ESCs requires the destruction of the embryos, which may give rise to ethical concerns (46). iPSCs derived from differentiated cells may obviate these ethical issues. But, as they are pluripotent stem cells, the problem of forming teratoma during proliferation and differentiation remains unsolved. Furthermore, there are serious problems in the process of inducing iPSC formation (47).
One of the advantages of SMILE is the smaller incision. “We’re defaulted to a 4-mm incision in the United States,” Dr. Manche explains. “In other countries, it’s even smaller. This small incision provides less transection of the nerves in the cornea, and that’s directly correlated to how denervated the cornea becomes, and also how much dry eye the patient experiences, especially in the early postoperative period. Typically, there’s less induced dry eye with SMILE compared with LASIK because LASIK requires a 270-degree circumference flap. With LASIK surgery, you’re severing all of the nerves in that area, which leads to relative denervation of the cornea. Typically, corneal reinnervation takes place over the course of six to 12 months. Another advantage to SMILE is that there are no flap complications.”
Tenocytes are derived from tendon progenitor cells, which are called tendon-derived stem cells (TDSCs) (18). TDSCs are a type of stem cell that possess some characteristics of multipotent stem cells (19). Defined by the specific stem-cell niche, MSCs can be classified into bone marrow-derived mesenchymal stromal cells (BMSCs), adipose-derived stem cells (ADSCs), TDSCs, and other sources of MSCs (20). These MSC-derived stem cells can be differentiated into tenocytes under appropriate stimulation in vitro.
At the five-year follow-up, all eyes in both groups were within 1 D of attempted spherical equivalent refraction, and no statistically significant difference was found between the intended and achieved correction comparing the groups at any time points.
ADSCs are advantageous in tissue engineering due to their multipotency, high proliferation, easily isolated amounts of cells from the subcutaneous tissue, and low donor site morbidity (82,83). ADSCs have been regarded as one type of seed cell for tendon tissue engineering that can differentiate into tenocytes in vivo and increase the tensile strength of the repaired tendon (84,85). However, their innate tendency towards adipogenesis may hinder the application of ADSCs in tendon regeneration (1,86). For this purpose, intense research was conducted to overcome this obstacle. Yu et al. confirmed that hypoxia or activating the expression of hypoxia-inducible factor-1 could improve the tenogenesis of ADSCs (87). Additionally, several studies have indicated that the supplementation of growth factors could improve cell proliferation of ADSCs and promote tendon repair efficiency (88-90). Tendon ECM components (91) and TNMD (92) enhance the proliferation and tenogenesis of ADSCs. Physical stimulation such as uniaxial tensile cyclic loading (2% strain and 0.1 Hz frequency) (93) and extracorporeal shock waves in tenogenic medium (94) can also boost the differentiation of human ADSCs toward tendon-like cells.
ESCs can give rise to all tissues derived from the three germ layers (53). Because of this, ESCs hold great promise as seed cells for tendon tissue engineering (54). Thus, how to differentiate them into the tendon lineage has become a key point. Some researchers have investigated a stepwise differentiation approach by first inducing human ESCs to differentiate into MSCs, and subsequently allowing the MSCs to form tendon-like tissues. The results in vivo and in vitro showed that human ESC-derived MSCs exhibited tenocyte-like morphology and positively expressed tendon-related gene markers such as Scx, col I and col III, as well as other mechano-sensory structures and molecules (55,56). Moreover, the formation of teratomas could be avoided if ESCs are induced into MSCs before the transplantation (55). In addition, they demonstrated that the use of dynamic mechanical stress (1 HZ, 10% for 2 h/day) and bone morphogenetic protein (BMP)12 and BMP13 could promote differentiation of human ESCs into tenocytes (57-60).
Published by AME Publishing Company Address: Flat/RM C 16F, Kings Wing Plaza 1, NO. 3 on Kwan Street, Shatin, NT, Hong Kong, China.Email: editor@atmjournal.org
The cells in the human body can be divided into two categories based on their differentiation status (Table 1). One is differentiated cells, such as tenocytes and dermal fibroblasts, which lack self-renewal capability in vivo. Differentiated tenocytes and dermal fibroblasts can be expanded in vitro in the presence of serum but have a limited expansion capacity. Culturing in vitro with the supplementation of growth factors may activate their ability of proliferation, but these cells still lack the capacity of differentiating into other cell types. Besides, their phenotype may change, which will cause a deficiency in their functions with increasing passaging (18). The other is stem cells, which can replicate themselves as well as differentiate into specialized cells under appropriate conditions (22). At the same time, their ability to proliferate and differentiate is difficult to control in vivo, which makes them susceptible to forming of tumor and undesired tissue cells during differentiation.
Moshaverinia et al. tested the capacity of encapsulated dental MSCs to differentiate into tendon tissue in vitro and in vivo. Their findings indicate that periodontal ligament and gingival tissue-derived MSCs can be considered as suitable stem cell sources for tendon engineering (104). Chen et al. explored dental pulp stem cells (DPSCs) for potential application in tendon tissue engineering and found that mature tendon-like tissue was formed after transplantation of DPSCs in a special fiber scaffold constructs under mechanical loading in a mouse model (105).
For example, a retrospective case series from Turkey found that SMILE and FS-LASIK were safe and similar in terms of efficacy and predictability at five-year follow-up for the correction of myopia and myopic astigmatism.1 The study included 44 eyes from 22 patients who received SMILE in one eye and FS-LASIK in the contralateral eye. Patients were examined at one, three and five years.
Dr. Manche agrees. “In all fairness, SMILE is relatively new, and it’s really quite impressive how good the data are this early in the evolution of the procedure,” he says. “I think it’ll just get better with time.”
Human embryonic development begins with the cleavage of the fertilized egg. It then divides into many smaller cells leading to the formation of the blastula. Through the cell movements of gastrulation, the embryo is rearranged to form the three main germ layers: the ectoderm, mesoderm, and endoderm. The mesoderm then gives rise to chordamesoderm, paraxial mesoderm, intermediate mesoderm, and lateral plate mesoderm. With the establishment of body axes and formation of the neural tube, limb buds arise from lateral plate mesoderm at the appropriate levels along the ventral domain of the body (10). The early limb bud has two major components: an outer layer of ectodermal epithelial cells, and a core of loose undifferentiated mesenchymal cells derived from the lateral plate mesoderm (11,12). The skeletal elements and connective tissues (including tendon structure) of the limb develop from these mesenchyme cells, but the limb muscles are derived from the somites which stem from the region of paraxial mesoderm and migrate into the limb bud. Therefore, the origin of tendon tissue is the same as that of bones, cartilage, and any other connective tissues, but not muscle. Analysis of the expression of scleraxis (Scx), a tendon specific transcription factor, revealed that the limb tendon progenitors originate from the subectodermal mesenchyme in proximomedial domains of the limb bud (13). Regulated by multiple morphogens and growth factors, three pairs of tendon primordium appear in a proximo-distal sequence in the developing limb (14,15). Proximal and intermediate tendon primordium appears the earliest on the dorsal side around limb junction. Following closely, intermediate tendon primordium appears on the ventral side around intermediate limb junction. The ventral proximal tendon primordium forms after the appearance of ventral intermediate tendon primordium. Subsequently, distal tendon primordium appears at both the dorsal and ventral sides of the distal limb. After the stimulation of growth factors and mechanical stress (16), the three pairs of tendon primordium will then differentiate into adult tendon structure in a proximal-to-distal sequence in the developing limb (Figure 1).
Unusual Fire and Explosion Hazards: When heated to decomposition, zinc selenide may emit toxic fumes of selenium and oxides of zinc. On contact with strong ...




 Ms.Cici
Ms.Cici 
 8618319014500
8618319014500