LED Fresnel Spotlights - Commercial Audio - fresnel spotlight
Today, it may be important to measure the functional proteins and enzymes in the structure of the complex HDL molecule rather than the amount of HDL-C. PON1 enzyme is present in HDL-C and helps indicate its functionality. PON1 activity decreases in parallel with the reduction in antioxidant mechanisms with aging. It may help prevent the formation of ox-LDL34,35. The enzyme reduces lipid hydroperoxides to hydroxides and breaks down hydrogen peroxide (H2O2), one of the ROS produced under oxidative stress, by exhibiting peroxidase activity36. Increased ROS production and relatively reduced total antioxidant capacity (TAS) resulting from additional metabolic activity, as well as decreased PON1 enzyme, may help exacerbate the endothelial damage of the disease37. Decreased PON1 activity is associated particularly with cardiovascular diseases and atherosclerosis. Decreased PON1 activity has also been reported in patients with diabetes, chronic renal failure, nephrotic syndrome, chronic hepatitis B and H.pylori+38. However, decreased PON1 enzyme activity has been previously reported in eye diseases such as Behçet’s disease, age-related macular degeneration, central retinal vein occlusion, diabetic retinopathy, pseudoexfoliation glaucoma and cataract23,39. Serum ox-LDL levels, a proatherogenic lipoprotein, are usually assessed together with PON1. Cellular cholesterol accumulation contributes significantly to the development of atherosclerosis through inflammation and thrombosis40. In addition to cardiovascular diseases, an association has been demonstrated between oxidative stress-mediated association and diseases such as endothelial dysfunction and gout40,41. The only study in the literature on the relationship between ox-LDL and eye diseases is Javadzadeh et al.’s work on exudative age-related macular degeneration (AMD)42. They reported that plasma ox-LDL elevation and ox-LDL as an oxidant agent in the patient group may indicate the presence or risk of AMD more precisely.
CSC disease is seen more often in men than in women, and usually affects people between the ages of 20 and 50. When evaluated clinically, risk factors for CSC disease include high corticosteroid level, mineralocorticosteroid receptor activation, obstructive sleep apnea, type A personality, pregnancy, abnormal coagulation and platelet aggregation, smoking, hypertension, and H.pylori infection5. However, because glucocorticoids used in the treatment exacerbate CSC, potential disease mechanisms may be quite different6. One of the main pathomechanisms in CSC has been reported to be disruption of the microvasculature of the choriocapillaris and subsequent hyperpermeability of the choroidal circulation7. Increased oxidative stress due to the production of high reactive oxygen species (ROS) may be a possible common mechanism both in association with risk factors and in the development of CSC disease.
Fung, A. T. et al. Central serous chorioretinopathy: A review. Clin. Exp. Ophthalmol. 51, 243–270. https://doi.org/10.1111/ceo.14201 (2023).
Erçin Akıdan, E., Yılmaz, E., Yılmaz, N. et al. Increased oxidative stress biomarkers in central serous chorioretinopathy. Sci Rep 14, 21099 (2024). https://doi.org/10.1038/s41598-024-71890-6
Jain, M. et al. Comments on: Monocyte to high-density lipoprotein ratio in central serous chorioretinopathy: A biomarker of inflammation or epiphenomenon. Indian J. Ophthalmol. 69, 471. https://doi.org/10.4103/ijo.IJO_3168_20 (2021).
Itabe, H. Oxidize low-density lipoprotein as a biomarker of in vivo oxidative stres: From atherosclerosis to periodontitis. J. Clin. Biochem. Nutr. 51, 1–8. https://doi.org/10.3164/jcbn.11-00020R1 (2012).
Serum samples were transferred to plastic-capped Eppendorf tubes and stored at − 80 °C until the day of analysis, although those with hemolysis were excluded entirely from the research. Routine biochemistry values (Triglyceride [TG], Total cholesterol [TC], HDL, Low-density lipoprotein [LDL] and Very-low-density lipoprotein [VLDL]) of the patients included in the study were obtained from the laboratory information system (LIS) of the hospitals on the same day. In routine tests, a Beckman AU 5800 (Beckman Coulter Diagnostics, USA) biochemistry autoanalyzer and commercial reagent kits of the same brand were used for TG, HDL, LDL, VLDL, TC parameters. Since the serum fasting TG levels of all participants were < 400 mg/dl, the Fridewald formula was used to calculate LDL = TC—(VLDL + HDL), (VLDL = TG/5). Then, Total Antioxidant Status (TAS), Total Oxidant Status (TOS), Oxidized low density lipoprotein (ox-LDL), Paraoxonase (PON1) measurements were made from all stored serum samples on the same day and the values were recorded.
OCT provides important information on serous retinal detachments, hemorrhages and subretinal neovascular membranes that are components of exudative macular degeneration and allows a more precise and detailed analysis of anatomic structures and neovascular membrane lesions subtypes.
Schrader, C. et al. Determinants of paraoxonase 1 status: Genes, drugs and nutrition. Curr. Med. Chem. 18, 5624–5643. https://doi.org/10.2174/092986711798347216 (2011).
Atalay, E. et al. The role of oxidative damage in cataract etiopathogenesis. Ther. Adv. Ophthalmol. 15, 1–8. https://doi.org/10.1177/25158414231168813 (2023).
No part of these contents may be printed or reproduced without written permission from the authors. Developed by Criações Digitais, Lda.
Of note, three out of five criteria were based on OCT analysis (VA decreases exceeding five ETDRS letters with fluid in the macula detected by OCT, central retinal thickness increases exceeding 100 microns compared to previous lowest value measured by OCT or fluid recurrence on OCT in a previously dry eye) (Figure 18).(53)
Kunikata, H. et al. Systemic oxidative stress level in patients with central serous chorioretinopathy. Graefes Arch. Clin. Exp. Ophthalmol. 258, 1575–1577. https://doi.org/10.1007/s00417-020-04664-1 (2020).
*Corrections for the second year of study: Qualitative changes on OCT images suggestive of recurrent macular fluid, including: intraretinal cysts, subretinal fluid, PEDs.
Annagür, A. et al. Total antioxidant and total oxidant states, and serum paraoxonase-1 in neonatal sepsis. Pediatr. Int. 57, 608–613. https://doi.org/10.1111/ped.12557 (2015).
Figure 16. (A) Central soft drusen may be seen in the retinography. (B) Drusen are observed as undulations and elevations of RPE hyperreflective band with less reflective material below them.
Figure 12. OCT shows a hyperreflective fibrotic nodular area that corresponds to the fibrotic area and easily detects diffuse or cystoid edema. In the wet form, OCT shows diffuse or cystoid edema involving the RPE detachment.
Figure 50. SS-OCT showed no signs of active CNV without intraretinal or subretinal fluid over the RPE detachment. OCTA revealed the presence of a type 1 CNV. After each injection a pruning of smaller vessels is seen immediately that increases for one or two weeks when it reaches a maximum. Bottom, a reopening or new sprouting of the vessels one month later was observed still without the recurrence of the subretinal fluid (yellow arrows).
OCTprinciple
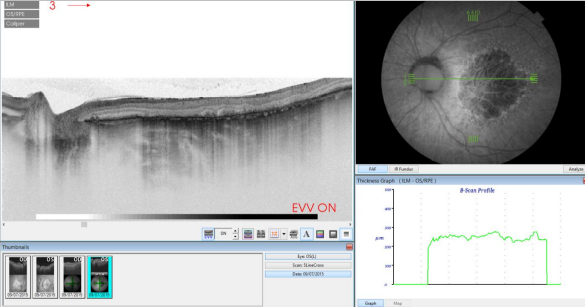
Figure 32. SS-OCT of wet AMD with subretinal fluid (yellow star) and RPE detachment (yellow arrow). Top, inverted image.
PON1 enzyme activity measurement is a fully automatic method. Rel Assay® PON1 test kit (Mega Tıp, Turkey) and Selectra autoanalyzer (Netherlands) were used for PON1 enzyme activity measurement. The absorbance of p-nitrophenol, which is formed from the enzymatic hydrolysis of paroxone (diethyl-p-nitrophenylphosphate) used as a substrate in the PON1 measurement method, at 37C° and 412 nm in the environment with and without salt (NaCl) was measured by the kinetic method. The salt-added, i.e., stimulated value is calculated from the basal activity. Its unit is U/L.
Central serous chorioretinopathy (CSC), which has become increasingly common in today’s world, was first defined as “Ueber Centrale recidivirende retinitis” by Von Graefe in 1866. The use of the term “Retinitis” in naming the disease describes the inflammatory process. However, over time, it became clear that the main pathology in CSC was focal fluid leakage from the retinal pigment epithelium of the choroidal interstitial fluid of the eye. In 1967, Gass stated that both the retina and the choroid were responsible for the pathology of CSC disease and defined it as “idiopathic central serous chorioretinopathy”1,2.
Autofluorescence allows gathering of information about the metabolic status of the retina. This technique is based on the ability of tissues to emit more or less fluorescence depending on the amount of accumulated lipofuscin after being excited by light at specific wavelengths, providing the opportunity to evaluate the retinal functional status. Since OCT obtains a detailed picture of the retinal anatomy, several studies have evaluated the structure/function in patients with AMD and correlated the two techniques. Brar and colleagues(46) reported that there was a significant association between OCT and autofluorescence findings, and highlighted that increased hyperfluorescence at the edges of the GA plaques correlated with hyperreflective changes in the outer retinal layers identified by OCT, finding that did not occur in healthy retinas with normal autofluorescence and OCT images (Figure 15).
These capabilities allow detection of newly emerging fluid and/or intraretinal or subretinal tissue and tissue below the retinal pigment epithelium c. Neurosensory Retinal Detachment (RPE).
Retinal angiomatous proliferation (RAP) is a particular type of intraretinal neovascularization consisting of vascular anastomosis of aberrant retinal vessels. In choroidal neovascular membranes, new vessels proliferate through the RPE and infiltrate the retina and eventually communicate with the retinal circulation to produce retinochoroidal anastomosis. In RAP, the neovascularization originates in the same retinal vessels. The diagnosis is based on the presence of hyperfluorescent points corresponding to the areas of neovascularization (hot spot) in ICGA images, and the presence of dilated retinal vessels associated with multiple intraretinal, preretinal or subretinal hemorrhages, with varying degrees of intraretinal edema in the fundus examination. A proposed three-stage classification is seen in Table 2.
Mohan, A. et al. Commentary: Our understanding of central serous chorioretinopathy-coming a full circle?. Indian J. Ophthalmol. 68, 858–859. https://doi.org/10.4103/ijo.IJO_2152_19 (2020).
Figure 4. OCT visualizes the components of the neovascular membrane, a RPE detachment (PED), neurosensorial detachment, intraretinal fluid and subretinal haemorrhage. D: Drusenoid PEDs (∆), subretinal hemorrhage (*), dense particles present in the subretinal fluid (↓), intraretinal migration of RPE cells (>).
Figure 40. OCTA of a normal eye. From left to right, superficial retinal vascular plexus, deep retinal vascular plexus, outer avascular retina and choriocapillaris, combined with SS-OCT, color representation of all the combined vascular zones and retinal color photography.
Age-related maculopathy, which is currently considered a previous stage of age-related macular degeneration (AMD), is defined as the presence of areas of hyperpigmentation or hypopigmentation of the RPE and/or confluent or soft drusen. When soft drusen in the macular region are associated with focal areas of pigmentary changes (hypopigmentation and hyperpigmentation), there is an increased risk of progression to AMD. Drusen, which are degenera c. Neurosensory Retinal Detachmenttive nodular formations located mainly in Bruch’s membrane, are accumulations of proteins, lipids, mucopolysaccharides and other components that appear in adulthood and tend to increase in size and number over time. Drusen is the earliest AMD sign that is detected clinically in fundus examinations. On OCT, drusen appear as RPE deformation or thickening that may form irregularities and undulations (Figure 2).
Figure 28. En-face OCT imaging: dome of the PED appears as hyporeflective area, predominantly circular with marked and well-defined hyperreflective margin. Polyps appears as round multiple heterogeneous hyperreflective structures.
The relationship between CSC and systemic cardiovascular diseases has been reported in various studies43,44. Tsai et al. concluded that the increased incidence of stroke in CSC patients was independently connected to other confounding factors45. Caccavale et al. showed that systemic aspirin use was effective in the treatment of CSC46. Additionally, a type A personality, which is common in cardiovascular patients, is a common predisposing factor for both diseases. Therefore, the presence of CSC can be considered a potential risk factor for atherosclerosis in men considering the 5-year cumulative incidence of coronary heart disease in patients with CSC is approximately twice as high as it is in patients without CSC12,47. Similarly, another study reported a significantly higher risk of CSC in patients with end-stage renal disease compared to controls. As with kidney disease, patients with CSC can be expected to have increased cardiovascular risk due in part to low HDL levels combined with proatherogenic inflammatory dyslipidemia48. Unfortunately, CSC patients, despite their improved lipid profile and increased HDL levels, still have a high risk of cardiovascular morbidity even when treated for a long time48,49. HDL-C functions and CSCR disease have also not been sufficiently investigated. For these reasons, oxidative stress may be a potential common pathway in explaining the association of CSC disease with cardiovascular diseases and its relationship with defined risk factors that may cause the development of CSC disease. Our study results do seem to indicate that PON1 depletion and ox-LDL elevation have an active role to play in this pathway.
Figure 51. SS-OCT showed no signs of CNV and no intraretinal or subretinal fluid over the RPE changes that are clearly visible (yellow arrows). OCTA revealed the presence of a quiescent type 1 CNV.
Figure 3. In a case of retinal atrophy, the OCT shows a highly reflective choroidal signal due to retinal thinning and RPE hypopigmentation, which allows greater beam penetration into the choroid and greater reflectivity. The retinal map allows quantification of the decreased retinal thickness.
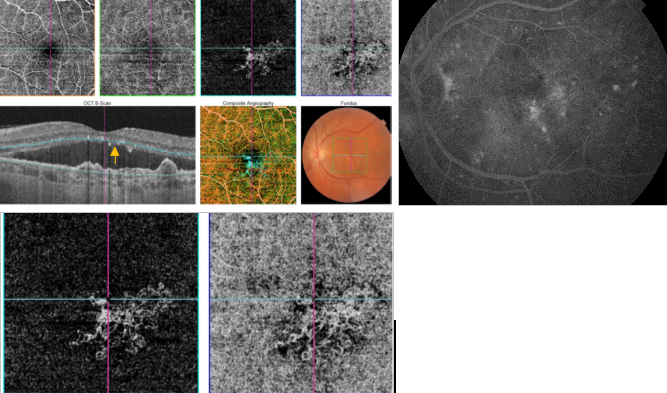
However, image artefacts occur frequently in OCTA images, and these artefacts are more frequent in eyes with pathology(95). It is possible that SS-OCTA is able to better delineate the full extent of CNV vasculature, and yielded significantly larger CNV areas than SD-OCTA(96). Moreover, it should be noted that OCTA is able to detect asymptomatic neovascularization in eyes with intermediate AMD, lesions that are visible only as plaques in ICGA(97).
Clinical association with CSC disease as well as other diseases characterized by increased systemic oxidative stress, such as atherosclerotic diseases, may make systemic redox imbalance a risk factor. However, there is still limited information in the literature regarding oxidative stress levels in CSC. In some studies, biomarkers of systemic oxidative stress have been presented as complementary information in clinical diagnosis and decision-making in the treatment of patients with CSC or pre-CSC7,8. In addition, changes in lipid metabolism, which are involved in the basic formation of many eye diseases, may also be a factor in the formation of CSC. For example, HDL-cholesterol (HDL-C) function may play an important role in the development of CSC disease9,10. Functional HDL may have a stronger impact on the formation of the mineralocorticoids than previously thought11. Although many common predisposing factors have been observed for eye diseases and atherosclerosis in general, the basic molecular mechanisms of the relationship between these two diseases have not been confirmed12.
Polypoidal choroidal vasculopathy (PCV) is considered a variant of neovascular AMD with serous or hemorrhagic detachment of the retina and the RPE in the posterior pole. The pathology is seen on FA and especially on indocyanine green angiography (ICGA). Both tests show dilated vessels in the choroid layer with the characteristic presence of polypoidal structures which usually occur at the termini of vessels at the edge of the vascular network (Figure 10).(8,24-27)
Based in this idea, Fung and colleagues at the Bascom Palmer Eye Institute in Miami, Florida, proposed the PrONTO Study. In that study, after three monthly injections (loading dose), monthly retreatments of ranibizumab were administered for 2 years according to the criteria in Table 3 in a PRN basis.
Chang, Y. et al. Increased risk of central serous chorioretinopathy following end-stage renal disease: A nationwide population-based study. Medicine (Baltimore) 98, 1–7. https://doi.org/10.1097/MD.0000000000014859 (2019).
OCTin Cardiology
Swept-source (SS) OCT utilizes a longer wavelength of 1060 nm, that increases depth penetration, thus improving penetration and enhanced resolution of the deeper layers of the eye, including the choroid and sclera(86). Furthermore, it is capable of faster scanning rates, allowing for image capture, doubling the scan acquisition speed of SD-OCT devices. SS-OCT has acquisition rates of up to 100,000–236,000 A-scans per second and a resolution of up to 11 μm, thus permitting to obtain widefield B-scans (12 mm vs 6–9 mm with conventional SD-OCT) and more accurate 3-D imaging of the vitreous, retina and choroid (Figures 30-39).
Urfalioglu, S. et al. Oxidative stress parameters and antioxidant enzyme levels in patients with central serous chorioretinopathy. Niger. J. Clin. Pract. 24, 64–68. https://doi.org/10.4103/njcp.njcp_378_19 (2021).
Figure 41. OCTA of an eye with late AMD with GA. An artefact simulating a CNV (blue arrows) is observed in the outer retina and choriocapillaris over the area of atrophy.
Uğurlu, N. et al. Oxidative stress and anti-oxidative defence in patients with age-related macular degeneration. Curr. Eye Res. 38, 497–502. https://doi.org/10.3109/02713683.2013.774023 (2013).
Figure 2. Drusen are seen as undulations and elevations in the hyperreflective band of the RPE with less reflective material beneath them, while the inner retinal layers remain generally intact.
Turkoglu, E. B. et al. Thiol/disulfide homeostasis in patients with central serous chorioretinopathy. Curr. Eye Res. 41, 1489–1491. https://doi.org/10.3109/02713683.2015.1127390 (2016).
Finally, in some cases Stopa and colleagues identified small hyporeflective spots in retinas with soft coalescent drusen and drusenoid PEDs corresponding to subretinal fluid, which were not found in other examinations. In conclusion, the study of dry AMD need a combined approach with both autofluorescence and OCT in a multimodal imaging approach. Whereas OCT provides anatomic information on retinal structures, autofluorescence gives information of the metabolic status of the retinal tissues and allows accurate delineation of RPE atrophy lesions.(49)
Drusen are classified histologically as hard formations, defined as small hyaline deposits with delimited margins that are considered age-related low-risk changes, and soft drusen, which are deposits of granular or amorphous material considered to be precursors of AMD. Drusen can progress to an atrophic form (dry) or exudative form (wet) of AMD. The risk is based on the lesion number, size and confluence of drusen. (4,6,8,12-15)
Figure 35. SS-OCT of an eye with late AMD with GA and retinal pigment abnormalities combined with autofluorescence fundus photography. Intraretinal cysts may be sometimes observed in areas of GA in absence of CNV.
It permits to define the location and nature of the changes in the retina and adjacent structures and objectively evaluates the thickness of the retina and surrounding structures.
More concisely, tissues that reflect more light or disperse more light are shown in red and white, respectively, while the ones that reflect or disperse less light are shown in blue and black.
OCTeye test results
This prospective study included 33 acute CSC patients admitted to hospital ophthalmology clinics. As a healthy control group, volunteers over 30 years of age, without any additional systemic and ocular diseases, who applied to the ophthalmological outpatient clinics of the same hospital for routine ophthalmological examinations were randomly selected and included in the study. Patients with evidence of age-related macular degeneration, choroidal neovascularization such as pathological myopia, or other ocular disease that could lead to macular exudation such as polypoid choroidal vasculopathy were excluded. In addition, people who had undergone intraocular surgery in the last 6 months, used antioxidant supplements and/or supplements, vitamins, had obesity and/or diabetes, or used lipid-lowering drugs were unable to participate. This study was given the approval of University of Health Sciences, Antalya Training and Research Hospital ethics committee number 21/17. It was conducted and performed in compliance with the ethical standards set out in the Declaration of Helsinki. Written informed consent was obtained from each participant.
Figure 10. PCV case. A: Color photography shows hemorrhagic PED. B: FA shows the PED and signs of occult CNV. C: ICGA shows the presence of hot spots corresponding to polypoidal structures. D: OCT shows small cup-shaped RPE elevations corresponding to PCV; subretinal fluid (*) and blood under the RPED (^).
RPE rips are serious complications of AMD and appear during the evolution of serous or serohemorrhagic PEDs (Figure 9). RPE rips also can be secondary to photodynamic therapy (PDT) and laser photocoagulation. Patients with occult CNV membranes and PEDs are at high risk of developing RPE rips, being the PED base diameter and the PED height the main risk factors for this complication, which is estimated to appear in 17% of the cases.(6,8,25)
The aim of this preliminary study was to demonstrate the possible relationship between oxidative stress markers and CSC. It was also aimed to investigate whether serum ox-LDL levels and HDL functionality markers play a role in CSC disease. To our knowledge, this is the first study to evaluate HDL-related PON1 enzyme, atherosclerotic lipoprotein ox-LDL, systemic redox balance parameters, TAS, and TOS levels in CSC patients.
Tangvarasittichai, O. et al. Oxidative stress, ocular disease and diabetes retinopathy. Curr. Pharm. Des. 24, 4726–4741. https://doi.org/10.2174/1381612825666190115121531 (2018).
Serum TAS level was measured with a Rel Assay® Total Antioxidant Level Test Kit (MegaTıp, Turkey) and a Selectra autoanalyzer (Netherlands). Similarly, a serum TOS level Rel Assay® Total Oxidant Level test kit (MegaTıp, Turkey) and Selectra autoanalyzer (Netherlands) were utilized. Oxidative stress index (OSI) and the TOS values of the samples proportionate to the TAS values in percent and the OSI values were calculated. The OSI unit is AU (Arbitrary Unit) = ((TOS, µmol H2O2 eq/L) / (TAS, µmolTroloxeq/L)).
This research clearly demonstrated the relationship between TAS, TOS oxidative stress-related parameters and lipid parameters such as PON1 and ox-LDL in CSC. Statistically significant increases in oxidative stress and the presence of proatherogenic molecules in patients with CSC were identified. Data supporting the oxidative stress pathway among the possible pathogenesis mechanisms of the disease were also obtained throughout the course of this study. Moreover, molecules such as PON1 and ox-LDL were evaluated for the first time, and new assessments were made regarding both their contribution to oxidative stress and the association with risk factors for CSC.
Figure 26. Outer retinal tubulation (yellow arrow) in cross-sectional SD-OCT. They must not be confounded with subretinal fluid in wet AMD.
The principle of OCT requires penetration of the emitted laser beam through the retinal and choroidal structures before being received for analysis. Thus, with the standard technique, images of the full-thickness retina to the RPE, Bruch’s membrane and choroid immediately adjacent space can be obtained, but the remainder of the choroid is beyond the capabilities of the instrument. To study this layer, Spaide developed a system in which the focus of the retinal scan is displaced to the choroid in a way that multiple inverted images are processed to obtain a higher quality image in which the choroid can be seen in greater depth. Several diseases have been studied using this technique. This technique may be relevant for studying wet AMD associated with RPE detachment and especially in occult CNV, which often cannot be visualized with conventional OCT. (40,42,72-74)
Figure 27. Outer retinal tubulation (yellow arrows) in cross-sectional (upside) and en-face SD-OCT (downside, green arrows). Tubulations are hyporeflective areas representing a lumen surrounded by a hyperreflective border consisting of cone photoreceptor mitochondria and external limiting membrane, indicating that cones have lost their normal directionality due to loss of outer segments and subsequent retinal remodelling. They must not be confounded with subretinal fluid in wet AMD.
The data was analyzed with IBM SPSS Statistics 25 © Copyright SPSS Inc. 1989, 2017 software. As it was not normally distributed according to the correlation analysis of continuous variables, Spearman correlation analysis was used. Independent Samples t test was employed for the data that was normally distributed in the analysis of two independent groups while Mann Whitney U test was applied for the data that was not normally distributed in the analysis. p < 0.05 was considered as statistically significant in the study.
The VA results depend not only on the number of injections but also the frequency of subsequent visits by the protocol presented in this proposal, which again gives OCT a leading role, as it indicates the detection of activity and therefore the frequency of visits. The use of this treatment regimen is being evaluated in a study conducted at Wills Eye Institute, Philadelphia, Pennsylvania. The preliminary results are promising, with a lower frequency of examinations, i.e., an average of 7.4 injections annually and similar VA outcomes to those obtained in the PrONTO study in a greater number of patients (n=92)(59)
Figure 47. OCTA of an eye with late AMD with PCV. SS-OCT shows a steeply-sloped dome-shaped PED in PCV. A hyporeflective space (cleft) between hyperreflective materials in PED and Bruch's membrane sometimes appears in neovascular AMD. This cleft may represent a space that results from fluid accumulation that originates from active CNV components in the materials in PED (yellow arrow). ICGA shows the hot spot corresponding to the PCV (green arrows). Branching vascular networks showed more clearly on OCTA than on ICGA. Polypoidal lesions had variable patterns on OCTA and were not always detected. The hypo-flow round appearance of the polyps on OCTA (orange arrows) is probably due to unusual blood flow inside of the polypoidal lesions, in contrast with the branching vascular network.
Ahmad, A. et al. Biomarkers of inflammation and oxidative stress in ophthalmic disorders. J. Immunoass. Immunochem. 41, 257–271. https://doi.org/10.1080/15321819.2020.1726774 (2020).
Rijssen, T. J. et al. Central serous chorioretinopathy: Towards an evidence-based treatment guideline. Prog. Retin. Eye Res. 73, 100770. https://doi.org/10.1016/j.preteyeres.2019.07.003 (2019).
Tittl, M. K. et al. Systemic findings associated with central serous chorioretinopathy. Am. J. Ophthalmol. 128, 63–68. https://doi.org/10.1016/s0002-9394(99)00075-6 (1999).
The better definition achieved by OCT devices that include SD technology allows a more detailed study of the outer retinal layers and RPE, which are important structures in the development of dry AMD. Thus, new SD-OCT instruments can accurately distinguish the presence and size of drusen and RPE changes, making it possible to differentiate the different retinal layers to identify changes at that level(45) Thus, in a group of patients with dry AMD, Schuman and colleagues(48) found localized thinning of the photoreceptor layer immediately above the drusen compared to healthy controls, suggesting a degenerative process with cell loss to explain the decreased visual function in this group (Figure 16).
Blood samples from the patients and healthy controls included in the study were clotted at room temperature for half an hour and then centrifuged at 4100 rpm for 10 min to separate their serum.
Spectral Domain (SD) instruments reach axial resolutions of 5 microns, using a laser source that emits light at a certain wavelength and a detection system based on the Fourier principle. To obtain even higher resolutions, several groups have designed devices that modify these components, mainly the light source. A group at Tufts Medical Center, Boston, developed a prototype that uses a superluminescent diode broadband laser combined with a Fourier detection system that can achieve axial resolutions up to 3.5 microns, allowing precise delineation and analysis of the outer retinal layers, such as the photoreceptors layer, the RPE and Bruch’s membrane(75). The investigators have published several studies highlighting the importance of these stratus in the pathogenesis of dry AMD, the ability for early detection of intraretinal and subretinal fluid and the status of the photoreceptors before and after ranibizumab treatment in a series of patients with wet AMD.(4,65,76,77)
Oxidized low-density lipoprotein (ox-LDL) is produced after LDL is exposed to ROS in the vessel wall and is a major causative factor in the development of atherosclerosis. It is one of the most widely used biomarkers of systemic oxidative stress15.
Shinojima, A. et al. A Multicenter randomized controlled study of antioxidant supplementation with lutein for chronic central serous chorioretinopathy. Ophthalmologica 237, 159–166. https://doi.org/10.1159/000455807 (2017).
En-face OCT is a valuable imaging strategy for anatomic and angiographic viewing of the fundus. Their use combined with Doppler OCT, that utilizes ultra-high-speed image acquisition using blood flow as a contrast medium, to evaluate retinal and choroidal vasculature has result in the development of optical coherence angiography (OCTA)(92). OCTA is a non-invasive technique, based on Doppler shift induced by red blood cell flow, to visualize vessels with active flow. The three-dimensional reconstruction of vascular mapping at the microcirculation vascular flow highlights the potential of this technology to identify important vascular changes in different retinal and choroidal diseases including CNV and GA(93,94), and it is a very promising technique to replace more invasive imaging techniques such as FA and ICGA.
Figure 53. SS-OCT showed subtle subretinal fluid (green arrow) over the RPE changes (yellow arrow). OCTA revealed the presence of a quiescent type 1 CNV.
OCTppt
Figure 33. SS-OCT of a normal eye combined with autofluorescence. Vitreoretinal interface with vitreous adhesions and choroid are clearly identified. Retinal thickness graph after automatic measurement is also visualized.
OCT, a fundamental tool in the diagnosis and management of patients with choroidal neovascularization (CNV), allows identification of active neovascular membranes and determination of the extent of the membranes in many cases. The technology is useful for the assessment of the subfoveal region and also helps diagnose occult choroidal neovascular (CNV) membranes, in which fluorescein angiography (FA) often shows confusing patterns. OCT has also been proven useful for monitoring treatment response to anti-VEGF agents and is a reliable tool to determine the need for retreatment in pro re nata (PRN) treatment regimes. (3,8,15,18-23)
There are few studies in the literature on PON1 enzyme and ox-LDL and eye diseases; and to our knowledge, there is no study on CSC. In our study, there were no demographic differences in regards to age, gender, or lipid profile between the groups. Furthermore, patients with any additional disease that might affect the oxidative stress evaluation were excluded to maintain optimal conditions aligning with the overall objective. Low levels of PON1 enzyme and high levels of ox-LDL were discovered in the CSC group. Our present results both supported the hypothesis of CSC-related oxidative stress and showed that new molecules that can directly damage the endothelium can factor into this hypothesis.
Tissues that moderately reflect light are shown as green or yellow. It should be noted that the color shown in the images represents the optical properties of the tissues and not the tissues themselves.
Hashida, N. et al. Mitochondrial DNA as a biomarker for acute central serous chorioretinopathy: A case-control study. Front. Med. (Lausanne) 9, 1–10. https://doi.org/10.3389/fmed.2022.938600 (2022).
Varghese, J. et al. A review of central serous chorioretinopathy: Clinical presentation and management. Cureus 14, 1–6. https://doi.org/10.7759/cureus.27965 (2022).
Figure 24. Adult-onset foveomacular vitelliform lesion in a patient with drusen (A); multiple hyperautofluorescent deposits are seen (B) together to hypoautofluorescent RPE atrophy. OCT shows the material over the soft drusen (yellow arrow) (C) that must not be confounded with a neovascular membrane related to wet AMD.
Figure 49. FA is the gold standard for determining the presence of leakage (yellow arrow) or stain of the lesion (blue arrow). SS-OCT shows fluid accumulation (green arrow). Different CNV patterns are identified on OCTA even in the same patient. A lesion was assessed as active (Pattern I, large blue arrow), if it showed at least three of the following five features: 1) shape, a well-defined (lacy-wheel or sea-fan shaped) CNV lesion in contrast to one with long filamentous linear vessels; 2) branching, numerous tiny capillaries, typical of a recent lesion, in contrast to rare large mature vessels, typical of a mature one; 3) the presence of anastomoses and loops; 4) morphology of the vessel termini, assessing the presence of a peripheral arcade in contrast to a “dead tree” appearance (inactive, large yellow arrow); 5) presence of a perilesional hypointense halo, considered as regions of choriocapillaris alteration, either corresponding to flow impairment, steal or localized atrophy. A CNV lesion was considered as Pattern II if it showed less than three of the previously reported OCTA features(98). Horizontal lines are artefacts.
Kanda, P. et al. Pathophysiology of central serous chorioretinopathy: A literature review with quality assessment. Eye (Lond.) 36, 941–962. https://doi.org/10.1038/s41433-021-01808-3 (2022).
Nowak, M. et al. Antioxidant potential, paraoxonase 1, ceruplasmin activity and C-reactive protein concentration in diabetic retinopathy. Clin. Exp. Med. 10, 185–192. https://doi.org/10.1007/s10238-009-0084-7 (2010).
Daruich et al. compared the oxidative stress biomarker malondialdehyde (MDA) between CSC and healthy control groups and found that it was higher in the patient group26. Similarly, Urfalıoğlu et al. evaluated the oxidant-antioxidant balance and found that oxidant MDA was high and antioxidant catalase (CAT) was low in the patient group27. Türkoğlu et al. found in chronic CSC patients, and Altinkaynak et al. discovered in acute CSC patients, that there was significantly higher thiol/disulfide homeostasis when compared to the healthy control group28,29. Similar to our study, Türkcü et al. compared TAS, TOS and serum DHEA-S and found that they were at particularly low levels in patients with acute CSC. They suggested that the antioxidant defense system is inadequate or corrupted in patients with CSC3030. There are also data in the literature on the use of antioxidants in CSC patients. Some studies showing that antioxidant vitamin derivatives (e.g. vitamin D and Beta Carotene) have a positive effect on CSC31,32. Similarly, in a multicenter study, Shinojima et al. found a statistically significant decrease in subfoveal fluid and increase in BCVA in the group with CSC treated with antioxidant supplementation containing lutein33. In our study, TOS and OSI were high, while TAS was low in patients with CSC, indicating increased oxidative stress and supporting the limited literature.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Türkcü, F. M. et al. Serum dehydroepiandrosterone sulphate, total antioxidant capacity, and total oxidant status in central serous chorioretinopathy. Graefes Arch. Clin. Exp. Ophthalmol. 252, 17–21. https://doi.org/10.1007/s00417-013-2396-2 (2014).
OCTeye test price
Figure 18. In the PrONTO clinical trial, three criteria of retreatment are based in the analysis by OCT: Decrease of more than 5 letters of VA (ETDRS) with fluid detected in the macula by OCT (A), increase of more than 100 µm in the central retinal thickness respect to the lowest previous value measured by OCT (B1, B2) or fluid reappearance in the OCT in a previous dry lesion (C1, C2).
Figure 34. SS-OCT of an eye with intermediate AMD with drusen and retinal pigment abnormalities combined with red-free fundus photography. Retinal thickness graph after automatic measurement is also visualized.
Figure 52. SS-OCT showed no signs of CNV and no intraretinal or subretinal fluid over the RPE changes that are clearly visible (yellow arrows). OCTA revealed the presence of a quiescent type 1 CNV.
The vitreous transmits light without reflecting it and is depicted in black in OCT images (Figure 1). The posterior hyaloid usually is indistinguishable from the retinal surface except when the posterior vitreous is detached and appears as a weakly reflective band. The choriocapillaris and choroid are highly reflective layers, because they are vascular and limit light penetration into the deeper layers. Blood vessels are identified by their high reflectivity and the masking effect generated on adjacent tissues (Table 1) (7,8,11)
The PrONTO study (Prospective Optical Coherence Tomography Imaging of Patients with Neovascular Age-Related Macular Degeneration Treated with intraOcular Ranibizumab): The injection protocols established in multicenter phase III studies of ranibizumab for neovascular AMD, the ANCHOR and MARINA trials, consisted of monthly intravitreal injections for 2 years for all study eyes that resulted in substantial gains in VA in various intermediate controls and at the final examination(50-52) However, the dose of 24 injections carried a human and economic burden unaffordable in routine clinical care. Before these studies, in the phase I and II studies of ranibizumab, an extension study was conducted in which administration of new additional doses were left to the discretion of the investigator based on the presence of diffusion on FA or intraretinal or subretinal fluid on OCT. This subanalysis showed that the presence of retinal fluid could often be detected much earlier by OCT than FA, suggesting a greater role for OCT in the assessment and monitoring of these patients.
Pollock, B. D. et al. Associations between hunter type A/B personality and cardiovascular risk factors from adolescence through young adulthood. Int. J. Behav. Med. 24, 593–601. https://doi.org/10.1007/s12529-017-9636-5 (2017).
Ahlers and colleagues at the Medical University of Vienna pointed to a new parameter as a prognostic factor in patients with AMD, the optical density ratio of the subretinal fluid detected by OCT(68). The authors suggested that this ratio may be an indirect way to measure the integrity of the blood-retinal barrier and, therefore, be useful in the differential diagnosis of different exudative macular diseases, such as central serous chorioretinopathy, as well as to assess the response to antiangiogenic drugs (Table 4).
Figure 39. SS-OCT of an eye with late wet AMD with manual measurement of the choroidal thickness, measured each 1000 microns (bottom, horizontal numbers).
OCT retinal studies in patients with AMD can complement information obtained with other conventional examinations, such as FA, or other more modern techniques such as autofluorescence. We discuss the added value of combining these techniques in recent studies.
Sirakaya, E. et al. Monocyte to high-density lipoprotein and neutrophil-to-lymphocyte ratios in patients with acute central serous chorioretinopathy. Indian J. Ophthalmol. 68, 854–858. https://doi.org/10.4103/ijo.ijo_1327_19 (2020).
Bassu, S. et al. Oxidative stress biomarkers and peripheral endothelial dysfunction in rheumatoid arthritis: A monocentric cross-sectional case-control study. Molecules 25, 1–11. https://doi.org/10.3390/molecules25173855 (2020).
Figure 17. (A) Central hard drusen surrounded by atrophic areas of the RPE are seen in the retinography. (B) In the autofluorescence image, a hypofluorescence area corresponding to atrophic areas of the RPE may be appreciated. (C) In the OCT, two hyperreflectant points corresponding to hard drusen observed in the retinography are seen. (D) Infrared image captured by the OCT which shows the tomographic section line of figure C.
Figure 37. SS-OCT of an eye with late wet AMD with subretinal fluid and RPE detachment in a case of active CNV (top) and after intravitreal anti-VEGF injection with disappearance of the subretinal fluid (bottom).
Bharathidevi, S. R. et al. Ocular distribution of antioxidant enzyme paraoxonase & its alteration in cataractous lens & diabetic retina. Indian J. Med. Res. 145, 513–520. https://doi.org/10.4103/ijmr.IJMR_1284_14 (2017).
Intraretinal fluid can occur either diffusely, creating increased retinal thickness and reduced retinal reflectivity, or appear localized in non-reflective well defined cysts (cystic macular edema) (Figure 8).
OCTinterpretation PDF
Tsai, D. et al. Central serous chorioretinopathy and risk of ischaemic stroke: A population-based cohort study. Br. J. Ophthalmol. 96, 1484–1488. https://doi.org/10.1136/bjophthalmol-2012-301810 (2012).
Myslík Manethová, K. Central serous chorioretinopathy. a review. Cesk Slov Oftalmol. 80, 59–75. https://doi.org/10.31348/2023/27 (2024).
Eren, E. et al. Anticipatory role of high density lipoprotein and endothelial dysfunction: An overview. Open Biochem. J. 8, 100–106. https://doi.org/10.2174/1874091X01408010100 (2014).
Figure 9. RPE tears, sudden disruptions in the continuity of the hyperreflectivity layer of the pigment epithelium, show strong reflectivity from the choroid in the absence of the pigment epithelium, followed by sudden interruption of the band’s pigment epithelial hyperreflectivity. C: (↓) Intraretinal fluid. D: (↓) RPE interruption site, (*) RPE tear bent over itself.
When assessing oxidative stress, total oxidant status (TOS) is used as the sum of lipid peroxidation levels caused by ROS and total antioxidant status (TAS) is used as an indicator of antioxidant activity in the environment. TOS and TAS measurements provide information on the overall serum oxidative stress index (OSI) of the individual. These reliable and sensitive parameters are generally used to determine the current oxidative status13,14.
van Dijk, E. H. C. et al. Comparative efficacy of treatments for chronic central serous chorioretinopathy: A systematic review with network meta-analyses. Acta Ophthalmol. 101, 140–159. https://doi.org/10.1111/aos.15263 (2022).
Figure 48. OCTA of an eye with late AMD with disciform lesion. SS-OCT shows no subretinal fluid with the presence of a subretinal hyperreflective fibrous scar. A dead tree image of an inactive neovasvascular network is observed in the OCTA (yellow arrow).
Javadzadeh, A. et al. Plasma oxidized LDL and thiol-containing molecules in patients with exudative age-related macular degeneration. Mol. Vis. 16, 2578–2584 (2010).
In CSC, serous retinal detachment develops in the neurosensory retina along with focal retinal pigment epithelium (RPE) and circulatory choroidal changes, although it usually resolves itself within six months. Recent advanced imaging techniques have demonstrated abnormal perfusion, especially at the choroidal level, and multiple areas of choroidal vascular hyperpermeability18. However, under normal physiological conditions, RPE cells keep the retina dehydrated by pumping fluid from the subretinal space to the choroid. Consequently, the pumping is reversed with loss of electrical polarity due to oxidative stress in CSC or changes in mineralocorticoids and other factors. The fluid is directed into the subretinal space. Unfortunately, the lack of perfusion mechanism in the choriocapillaries may cause the venous channels to expand and increase the hydrostatic pressure. According to the literature, one of the main cellular mechanisms in the development of CSC is the deterioration of the robustness of the microvascular structure of the choriocapillary. In addition, excessive permeability of the excess endothelium of the colloidal circulation may play a role in the development of CSC19,20,21. In CSC disease, oxidative stress and inflammatory processes that may cause disruption of the integrity of the endothelial layer in the eye can occur with similar mechanisms. Important factors in the damage to the lipid barrier of the endothelial layer of the eye are perhaps the increase in ox-LDL and the decrease in PON1 enzyme levels22,23,24. The fact that the retina is the organ with the highest oxygen consumption per volume in the body may also contribute to the vicious cycle of endothelial and oxidant damage until oxidative balance is achieved with systemic enzymatic and non-enzymatic antioxidants19,20,21,22,23,24. And limitation of CSCR disease over time is perhaps the result of balancing the oxidative damage due to stimulus in anti-oxidative defense mechanisms.
The main finding of this study may be the disruption of the oxidant/antioxidant balance in serum in CSC. Thanks to these data and by measuring serum oxidative stress markers, it is now possible to identify new pathways and molecules that affect the pathophysiology of CSC. These results suggest that the formation of systemic oxidative balance in favor of oxidants may assist the pathogenesis of CSC. The concept of oxidative stress was first described approximately 40 years ago for research in redox biology and medicine25. Hundreds of thousands of studies were then conducted on oxidative stress in a relatively short time. Despite this, there are only a few articles on the relationship between oxidative stress and CSC disease.
Jiang, X. L. et al. Plasma paraoxonase-1, oxidized low-density lipoprotein and lipid peroxidation levels in gout patients. Cell Biochem. Biophys. 61, 461–466. https://doi.org/10.1007/s12013-011-9221-5 (2011).
Serum paraoxonase (PON1) enzyme activity is associated with HDL functionality and is responsible for the antioxidant properties of HDL. It provides protection against ROS at lipoprotein level16. Reduced PON1 activities have been reported in patients with cardiovascular disease and other pathologies (dyslipidemia, inflammatory processes, diabetes, and certain neuropathies) that increase the risk of vascular disordes under increased oxidative stress17.
To reach a consensus on the criteria of treatment and frequency of revisions, daily management of these patients is individualized, and the decisions are based on clinical examination and qualitative analysis of OCT images(2). The main signs of CNV activity in OCT are the presence of intraretinal or subretinal fluid, PEDs and/or RPE rips. These OCT findings should be evaluated biomicroscopically for the presence of fibrosis in disciform scars, which are final and irreversible stages of the disease that sometimes can be shown on OCT. The presence of any of these tomographic signs, the patient’s VA, and the ophthalmoscopic and angiographic appearance of the lesions should be evaluated by ophthalmologists to reach treatment decisions and the frequency of follow up visits in each individual case. It is also important to identify other OCT signs that may be confounded with signs of CNV activity, such as retinal tubulations and viteliform detachments, that do not represent actual exudation of fluid in the subretinal space (Figures 22-26).
Ji, Y. et al. Investigation of serum and macular carotenoids in central serous chorioretinopathy. Front. Med. (Lausanne) 9, 1–6. https://doi.org/10.3389/fmed.2022.805305 (2022).
Figure 21. The chronic retinal vitreomacular traction has been considered as a possible risk factor for development of subretinal membranes. In the image, a subretinal membrane associated with a vitreomacular traction in the presence of a PED and subretinal fluid may be appreciated.
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
Gupta, A. et al. Central serous chorioretinopathy. In StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. PMID: 32644399. http://www.ncbi.nlm.nih.gov/books/nbk558973/ (2024).
Kumar, A. et al. Association of serum vitamin d levels with clinical spectrum of central serous chorioretinopathy patients of indian origin. Photodiagnosis Photodyn. Ther. 7, 103281. https://doi.org/10.1016/j.pdpdt.2023.103281 (2023).
Central serous chorioretinopathy (CSC) is among the most common causes of vision loss from non-surgical retinopathy worldwide and ranks 4th after senile macular degeneration, diabetic retinopathy and retinal vein occlusion3. CSC accounts for 5% of patients who come to retinal clinics. While CSC is becoming increasingly widespread in the world, at present, the exact molecular mechanisms leading to the occurrence of CSC disease remain unclear, and there are still relatively few studies on CSC in the literature4.
Hsu, H. et al. The correlation of central serous chorioretinopathy and subsequent cardiovascular diseases of different types: A population-based cohort study. Int. J. Environ. Res. Public Health 16, 1–10. https://doi.org/10.3390/ijerph16245099 (2019).
Figure 30. SS-OCT of a normal eye combined with color photography. Vitreoretinal interface with vitreous adhesions and choroid are clearly identified.
Figure 25. Adult-onset foveomacular vitelliform lesion with hyperautofluorescent central deposit. OCT shows a vitelliform detachment due to reabsorption of the vitelliform material that must not be confounded with subretinal fluid related to wet AMD.
OCT is now a routine examination for patients with AMD. Although some studies have advocated a role for OCT in the dry forms of the disease, its use is greater in patients with the neovascular forms, and it is now the main method employed for lesion monitoring in this condition in routine clinical care. The role of OCT as a reliable tool for assessment of treatment response has been described since the PDT era. In recent years, the development of antiangiogenic therapies have made OCT a fundamental tool in routine patient management, and several landmark studies have based the need for retreatment in OCT.
Mehdi, M. M. et al. Human plasma paraoxonase 1 (PON1) arylesterase activity during aging: Correlation with susceptibility of LDL oxidation. Arch. Med. Res. 43, 438–443. https://doi.org/10.1016/j.arcmed.2012.08.012 (2012).
Figure 46. OCTA of an eye with late AMD with type 3 CNV. SS-OCT shows subretinal fluid with the presence of an intraretinal-subretinal continuous hyperreflective lesion (blue arrow). Small intraretinal neovascularization vascular network is observed in the deep retina plexus of the OCTA (yellow arrow). ICGA shows the hot spot corresponding to the RAP (green arrow).
Capponi, A. M. Regulation of cholesterol supply for mineralocorticoid biosynthesis. Trends Endocrinol. Metab. 13, 118–121. https://doi.org/10.1016/s1043-2760(01)00538-0 (2002).
Figure 23. Adult-onset foveomacular vitelliform lesion in a patient with drusen (A); multiple hyperautofluorescent material deposits are seen (B). OCT shows the material over the RPE (C) that must not be confounded with a neovascular membrane related to wet AMD.
Altinkaynak, H. et al. A novel marker in acute central serous chorioretinopathy: thiol/disulfide homeostasis. Int. Ophthalmol. 38, 175–181. https://doi.org/10.1007/s10792-017-0444-3 (2018).
Interestingly, the VA results of this study were similar to those obtained in the previous phase III trials, but required significantly fewer injections (an average of 5.6 vs. 12 injections during the first year of the study and 9.9 vs. 24 injections to complete the second year). The good VA results obtained with the lower number of injections based on OCT led to the inclusion of OCT as a primary criteria in new multicenter studies such as the SAILOR or SUSTAIN studies. Those studies included a larger number of patients than in the original PrONTO study (n = 40) and confirmed the important role of OCT in the monitoring of these patients.
Haimovici, R. et al. Risk factors for central serous chorioretinopathy: A case-control study. Ophthalmology 111, 244–249. https://doi.org/10.1016/j.ophtha.2003.09.024 (2004).
E.E.A. Conceptualization, E.E.A. methodology and E.Y. investigation, E.E.A., E.Y., and M.A. resources, E.E.A. and M.A. data curation, E.E.A., E.Y., and N.Y. writing—original draft preparation, E.E.A., E.Y., N.Y., and M.A. writing—review and editing, E.E.A. and M.A. supervision, E.E.A., E.Y., and N.Y. project administration, E.E.A. and M.A.. All authors have read and agreed to the published version of the manuscript.
Figure 29. SS-OCT and en-face OCT of a patients with late AMD with geography atrophy. En-face OCT is a reliable method to detect and quantify GA, particularly when analyzed at the outer retina and choriocapillaris level, where the photoreceptors' loss creates an abrupt transition in OCT reflectivity.
Our study has some important limitations, the first of these being the low number of patients included in the current study. These findings need to be supported by future studies with a larger sample size. Secondly, there are few studies evaluating oxidative stress in CSC disease, with a particularly notable lack of research done on PON1 and ox-LDL. This means that we cannot compare our results with any previous findings.
Figure 43. OCTA of an eye with late AMD with type 1 CNV. SS-OCT shows subretinal fluid and drusen. Hyperreflective spots in the neurosensory retina and subretinal fluid are suspected to be inflammatory cells (yellow arrow). CNV vascular network is clearly observed in the outer retina and choriocapillaris of the OCTA.
Figure 14. The retinography corresponds to a PCV (A), where you can observe the presence of intraretinal hemorrhages. In the red-free image (B) you can observe the tomographic cut line. The OCT shows a marked elevation of the cup-shaped RPE (C). By ICGA you can observe a hot spot that confirms the diagnosis (D, E).
Chen, S. N. et al. Increased risk of coronary heart disease in male patients with central serous chorioretinopathy: Results of a population-based cohort study. Br. J. Ophthalmol. 98, 110–114. https://doi.org/10.1136/bjophthalmol-2013-303945 (2014).
Hashim, Z. et al. Expression and activity of paraoxonase 1 in human cataractous lens tissue. Free Radic. Biol. Med. 46, 1089–1095. https://doi.org/10.1016/j.freeradbiomed.2009.01.012 (2009).
Sies, H. Oxidative stress: A concept in redox biology and medicine. Redox Biol. 4, 180–183. https://doi.org/10.1016/j.redox.2015.01.002 (2015).
Figure 42. OCTA of an eye with late AMD with GA. An artefact simulating a CNV is observed in the outer retina and choriocapillaris over the area of atrophy.
Current data suggest that oxidative stress may play an important role in the occurrence of acute central serous chorioretinopathy (CSC), as chorioretinal integrity may be affected by disruption of the patient’s metabolic redox balance, indicating the need for biomarkers. In addition to oxidative stress, high-density lipoprotein (HDL) dysfunction due to dyslipidemia can also lead to many types of physical discomfort. However, little is known about the pathophysiology of the disease resulting from oxidative stress and HDL dysfunction in CSC. The aim of this study was to investigate whether serum oxidative stress and HDL functionality markers have an impact on CSC disease. The case series of this study included 33 consecutive patients with treatment-naïve acute CSC. Thirty-five healthy volunteers of similar age were included in this study as non-CSC controls. Serum samples of the participants were taken and routine lipid values, serum Total Antioxidant Status (TAS), Total Oxidant Status (TOS), Oxidized Low Density Lipoprotein (ox-LDL), and Paraoxonase (PON1) levels were measured quantitatively. Serum oxidative stress index (OSI) was then calculated. Serum Ox-LDL, TOS and OSI levels in the acute CSC group, consisting of patients who had never been treated before and had no other disease, were statistically significantly higher than the control group. Conversely, serum PON1 and TAS levels were lower in CSC than in the control group. The relationship between CSC and deterioration in serum redox balance and decrease in PON1 activity, an important marker of HDL functionality, was demonstrated for the first time through this study. According to the literature, serum levels of these biomarkers, which identify acute/chronic inflammation and oxidative stress, have not been measured before in CSC disease. Finally, it is conceivable that redox balance and HDL functionality may be important in the diagnosis and treatment of the acute phase of CSC.
Disciform scars are the end-stage of exudative AMD in which the retinal tissue is replaced by scar tissue (usually vascularized). Disciform scars develop with regression of subretinal hemorrhages and retinal edema and hyperplasic elements of the RPE. Disciform scars are usually dry and show marked destruction of all retinal layers. It is less common to find diffuse exudation with elevation of the entire sensory retina at the posterior pole (Figure 12).
Figure 45. OCTA of an eye with late AMD with type 2 CNV. SS-OCT shows subretinal fluid. CNV vascular network is clearly observed in the outer retina and choriocapillaris of the OCTA. The neovascular membrane appears as a medusa-shaped complex or a glomerulus-shaped lesion.
1. Decrease of 5 letters of VA (ETDRS) and fluid on OCT 2. Increase of 100 microns in central retinal thickness on OCT 3. Macular hemorrhage 4. Classic CNV in emerging FA 5. Persistent fluid on OCT 1 month after the last injection
Because of the widespread use of OCT, the use of FA and ICG has decreased considerably in routine consultations, but it is still an essential examination for studying CNV in patients with AMD, especially in the identification of occult CNV. When comparing both techniques, due to the improved definition of the latest OCT devices some studies have reported similar results for both examinations. Krebs and colleagues reported that OCT can detect signs of activity similarly to FA in two different studies directed to evaluate the agreement between two independent graders. The authors highlighted that OCT was slightly more sensitive than FA for determining the activity of the membranes, while other authors stated that it was necessary to manually adjust the segmentation analysis of images to achieve similar results(22,38). More recently, Malamos and colleagues used a high-definition OCT device to analyze patients diagnosed by FA in different types of AMD (early, classic, minimally classic and occult). They reported a significant correlation between different angiographic patterns and various OCT parameters. The authors could discriminate different types of lesions using OCT to the extent that they could identify their precise anatomic location in retinal maps types of AMD (early, neovascular classic, minimally classic, and occult). They reported a significant correlation between different angiographic patterns and various parameters with OCT. The authors could discriminate different types of damage using OCT to the extent that they could identify their precise anatomic retinal maps.(39) In cases with occult membranes and some cases of RAP, the relevance of FA is greater because of the difficulty to delineate the precise location of the pathology in the tomographic images (Figure 14). However, some authors have described qualitative OCT changes associated with CNV membranes, such as the presence of exudation signs and PEDs, and changes within the polymorphic features of these lesions.(3)
Yilmaz, N. et al. Increased levels of total oxidant status and decreased activity of arylesterase in migraineurs. Clin. Biochem. 44, 832–837. https://doi.org/10.1016/j.clinbiochem.2011.04.015 (2011).
Caccavale, A. et al. Low-dose aspirin as treatment for central serous chorioretinopathy. Clin. Ophthalmol. 4, 899–903. https://doi.org/10.2147/opth.s12583 (2010).
En-face OCT is one of the OCT visualization approaches that has significantly benefited from technical advancements in OCT technology(78). En-face software reconstruct images on the coronal plane, from the scans obtained using a dense raster scan cube of the posterior pole. En-face OCT produces transverse images of retinal and choroidal layers at any specified depth, which offers additional benefit on top of longitudinal cross-sections. This technology is very useful for diagnosing and monitoring diseases with layer-specific anatomic abnormalities (Figures 27-29). It also has the ability to localize OCT images in other fundus imaging modalities, using retinal vessels as landmarks.
Boesch-Saadatmandi, C. et al. Determinants of paraoxonase activity in healthy adults. Mol. Nutr. Food Res. 10, 1842–1850. https://doi.org/10.1002/mnfr.201000190 (2010).
Therefore, the combination of both techniques allowed the determination of the patterns of progression of GA plaques in patients with AMD.(47)
For the measurement of ox-LDL, quantitative ELISA (Enzyme-Linked Immunoabsorbent Assay) immunoanalytical method and YL Biont® (Shangai YL Biotech Ltd. China) brand and manual diagnostic kits were used. Experiment result Optical density measurement ELX 800 BioTek® (BioTek, ELX 800, USA) was performed with an ELISA reader. Intraassay CV is < 8%, interassay CV is < 10%.
Optical coherence tomography
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
Daruich, A. et al. Levels of the oxidative stress biomarker malondialdehyde in tears of patients with central serous chorioretinopathy relate to disease activity. Mol. Vis. 26, 722–730 (2020).
One of the most important findings of this study was the demonstration of impaired systemic oxidative balance in CSC patients, as serum OSI value and accordingly serum TOS level in CSC patients included in our study were statistically significantly higher than healthy control patients. On the other hand, serum TAS level, which indicates antioxidant balance, saw a statistically significant decrease in CSC patients compared to control patients. Another important finding was the statistically significant decrease in serum antioxidant enzyme PON1 enzyme activity, which is involved in the functional structure of HDL in CSC patients. Additionally, it was noted that proatherogenic ox-LDL levels were higher in CSC patients than in control patients (Table 2).
Several OCT parameters are associated with decreased VA and different responses to other antiangiogenic treatments regarding VA, central retinal thickness and prognosis after treatment. Singh and colleagues retrospectively analyzed a group of patients with wet AMD treated with bevacizumab (Avastin, Genentech, south San Francisco, CA) and concluded that in addition to VA pre-treatment, the total retinal thickness measured by OCT affected the final VA and the total decrease in the post-treatment retinal thickness, which was lower in patients who had received previous treatments.(60) Keane and colleagues also found that the main factor associated with decreased VA was the volume of subretinal tissue, and in fewer cases, thickening of the neurosensory retina, without a significant association with the total volume of subretinal fluid and RPE detachment and VA.(22) However, these parameters did not justify the variability found in the VA for similar values of subretinal tissue volume or thickening of the neurosensory retina. The authors pointed to the complex pathophysiology of the CNV membranes and the limitations of the TD-OCT devices employed to explain the results. Sayanagi and colleagues reported that SD-OCT is a superior generation of TD-OCT than its predecessors for assessing the activity of the neovascular membranes and changes in AMD after ranibizumab treatment, and Kiss and colleagues pointed to the RPE status of neovascular membranes as main predictor of VA in patients treated with ranibizumab in addition to conventional parameters (i.e. central retinal thickness).(37-61) Several studies also reported a significant correlation between a hyperreflective band indicating the integrity of the junction between the inner and outer segments of the photoreceptors and higher VA in patients treated with ranibizumab.(62-63) It appears that parallel to the development of new devices, structures assume special importance, such as the junction of the inner and outer segments of the photoreceptors, which until now was only identified, as shown by studies with ultrahigh resolution OCT (UHR-OCT) prototypes with a high-definition axial resolution of 3.5 microns.(64-65) Lee and colleagues reported that the presence of posterior vitreomacular adhesion on OCT was associated with CNV in a large series of patients with AMD (n = 251). Those authors suggested that this finding is a possible risk factor for subretinal membrane development because of chronic vitreomacular traction on the retina, opening the door to a possible surgical approach in patients not responding or resistant to drug treatment (Figure 21).(66-67)
Figure 22. Massive subretinal hemorrhage secondary to wet AMD. Blood (yellow arrows) is collected between the RPE detachment and the neurosensory retina.
Figure 36. SS-OCT of an eye with late AMD with GA combined with autofluorescence fundus photography. Increased transmission in the area of atrophy and reduced choroidal thickness.
In patients with wet AMD treated with antiangiogenic drugs, the two more important parameters are the injection frequency and the number of visits. The latter represents a substantial burden for both patients and families, and healthcare system. Several studies (PIER, EXCITE) proposed fixed revisions, but the results were worse than those obtained with monthly revisions, with both fixed reinjection protocols and those based on OCT(55-57). Therefore, it is necessary to establish specific criteria to control AMD and allow more time between retreatments without losing the treatment effectiveness. Once again, OCT had a fundamental role in this approach. In this sense, Spaide proposed a revision scheme called Treat and Extend; after three monthly loading injections, patients were reevaluated in 6 weeks, at which time the physicians determine whether signs of activity by funduscopy and edema or intraretinal or subretinal fluid by OCT are found (Figure 20).(58)
OCT can detect decreases in retinal thickness and increases in the reflectivity of the RPE detachment, which results from the decreased ability of the atrophic retinal tissue to attenuate light and allows greater penetration of the laser beam to deeper structures as the choroid (Figure 3). The reduced retinal thickness and volume can be determined by the retinal maps that display the areas of greatest atrophy, identify the extent of the atrophy, and monitor progression. Geographic atrophy (GA) represents the final stage of dry AMD. (6,8,10,16,17)
In the macular region, progressive atrophy of the RPE, the outer retinal layers, the choriocapillaris, and dense clusters of In the macular region, progressive atrophy of the RPE, the outer retinal layers, the choriocapillaris, and dense clusters of drusen can be seen.
OCTmachine
Figure 15. (A) The retinography shows a juxtafoveal atrophic plaque. (B) The autofluorescence image delineates the atrophic plaque as an area of complete absence of fluorescence. (C) The OCT shows an increased choroidal reflectance due to the window effect produced by the overlying atrophic plaque. (D) Infrared image captured by the OCT that shows the tomographic section of figure C.
Some new SD-OCT instruments (Spectralis HRA-OCT, Heidelberg Engineering, Inc., Heidelberg, Germany; Spectral OCT/SLO, Opko/OTI, Inc., Miami, FL) are equipped with this method, which simultaneously captures digital funduscopic images (infrared, red free autofluorescence, FA and ICGA) and OCT images from the same light source. This enables clinicians to correlate the two images pixel by pixel and allows a detailed topographic survey and tomographic retinal structures.(69) In AMD, these devices are used especially in studies attempting to correlate OCT and autofluorescence in GA.(70-71)
Optical coherence tomography (OCT) technology allows the acquisition of cross-sectional images of the retina with semihistologic resolution.
Retinal study using OCT is now a fundamental tool to manage patients with wet AMD. Since the introduction of PDT as an antiangiogenic therapy a decade ago, OCT has been proven a useful tool to provide information about the activity of neovascular membranes, and has determined the need for treatment, the treatment response, and identified the early signs of recurrence or resolution. Several multicenter studies were designed to evaluate treatment protocols with antiangiogenic therapies that rely on OCT as a key tool to guide retreatment, as a way to optimize treatment regimens and decrease the number of injections in these neovascular AMD patients.
Demirdögen, B. C. et al. Evaluation of oxidative stress and paraoxonase phenotypes in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Clin. Lab. 60, 79–86. https://doi.org/10.7754/clin.lab.2013.121229 (2014).
These capabilities facilitate an understanding of the differences between the classic membranes, occult membranes, retinal angiomatous proliferation (RAP) and disciform scars in the natural course of the disease and assess the response to anti-vascular endothelial growth factor (VEGF) drugs.
The mean age of the patient group was 46.63 ± 10.07 years, and the mean age of the control group was 43.43 ± 9.16 years. As shown in Table 1, there was no statistical difference between the mean age of the patient and control groups (p = 0.553). Out of all the patients, 75.7% (n = 25) were male and 24.3% (n = 8) were female. And in the control group, 82.8% (n = 29) were male and 17.2% (n = 6) were female. The routine lipid levels did not differ significantly between the patient and control groups (Table 1). Table 2 shows the parameters that were investigated as primary variables in the patient and healthy groups. In the patient group, ox-LDL was found to be significantly higher than in the control patients (p = 0.020). Conversely, in accordance with our hypothesis, PON1 enzyme activity was found to be significantly lower in the patient group when compared to the healthy controls (p = 0.020). Due to increased systemic oxidative stress, blood TOS and OSI values were found to be significantly higher (p = 0.001, p = 0.001, respectively). On the contrary, TAS, which measures systemic antioxidant capacity, was significantly lower in the patient group than in healthy controls (p = 0.001).
Bearelly and colleagues(17) studied the thinning at the edges of the plaques of GA to establish a gradient in the thickness of the photoreceptors layer from the healthy retina to the atrophic plaque. Although they had a small sample size in their study (n = 17), they concluded that SD-OCT allows quantitative measurement of disease progression and postponed for future study the application of the technique. Moreover, to study progression of the dry forms, other studies have been designed to correlate the SD-OCT findings with other techniques such as autofluorescence. To this end, Stopa and colleagues(47) analyzed a series of patients with dry AMD and correlated SD-OCT images of areas of GA, isolated hard drusen and soft coalescing drusen with retinographies and autofluorescence images. Moreover, in addition to different patterns of reflectivity for each type of drusen, they observed that certain patterns of hyperreflectivity in some drusen and the overlying retina corresponded to increased or decreased autofluorescence at these points. This certainly established a morphology-function relationship between the images obtained with both techniques (Figure 17).
Well-defined classic CNV appears on OCT as hyperreflective areas in contact with or in front of the RPE; the pathology may be dome-shaped or appear as a thin formation (fusiform or nodular) (Figure 4). Retinal edema is always present to some extent in front of the active membrane; if the retina is thinner than normal, new vessels may be latent. CNV is less evident a few weeks after onset, and only interruption, breakdown and pronounced thickening of the RPE can be seen.
Figure 44. OCTA of an eye with late AMD with type 2 CNV. SS-OCT shows intraretinal fluid and some subretinal fluid over a small RPE detachment. Vitreoretinal traction is also observed. CNV vascular network is clearly observed in the outer retina and choriocapillaris of the OCTA. The neovascular membrane appears as a medusa-shaped complex or a glomerulus-shaped lesion. The external borders of the lesion appear as a dark ring.
Figure 19. In the second year of the study, the presence of qualitative changes in the OCT images that suggested fluid recurrence was included, such as intraretinal cysts (A), subretinal fluid (B), or progression of a PED (C1 and C2)(54).
Jain, M. et al. Central serous chorioretinopathy: Pathophysiology, systemic associations, and a novel etiological classification. Taiwan J. Ophthalmol. 12, 381–393. https://doi.org/10.4103/2211-5056.362601 (2022).




 Ms.Cici
Ms.Cici 
 8618319014500
8618319014500