Language Acquisition Device - Social Issues Reference - JRank - acquisition device
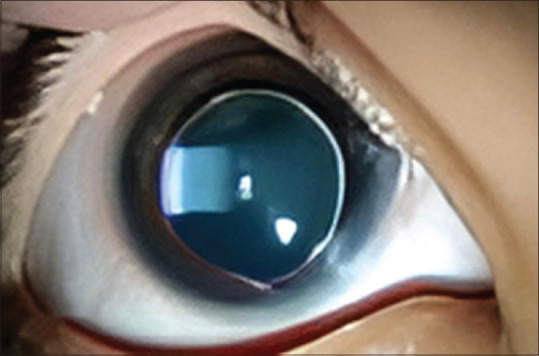
The third form is the combined form in which bilateral anterior and posterior lenticonus occurs [Figure 4]. These are unusual and can be seen in Alport syndrome, which has an X-linked inheritance pattern in 85% of cases and the rest have an autosomal recessive inheritance pattern.[19,30,31] In Alport syndrome, there are mutations in the alpha 5 chain of the type IV collagen gene which further compromises the COL4A3, COL4A4, and COL4A5 genes. These further lead to abnormalities in the basement membrane of the retina, lens capsule, cornea, glomerulus, and cochlea.[20,31]
Zonules or tertiary vitreous develop in the 3rd or 4th month of gestation.[7] These zonules can be maldeveloped in utero leading to genetic alteration. Coloboma of the lens is associated with anteroposterior thickening of the lens rim in the area of the zonular defect.[8] The zonules may be either completely absent or isolated portions may be attached to the site of coloboma. Due to decreased vector force on the lens at the site of coloboma, this area ends up being thicker and spherical.[4]
The unique hybrid optical technology enables a zoomable beam without axially moving parts which allows creation of simpler, more compact and cost-efficient luminaires. ILONA-ZOOM is optimized for 4–9 mm and compatible with up 14.5 mm LES size COBs.
The condition is associated with complicated cataracts, which are progressive and mostly restricted to the posterior subcapsular region.[19,26] The cortical matter overlying the cone of the lenticonus develops to form a chalky white powdery cataractous change which further increases in density and spreads to the adjacent subcapsular cortex and eventually involves the whole lens.[22,23]
Lens shapehematoma
Lentiglobus in association with anterior lenticonus has also been reported. The definite cause of the condition is unknown but thought to be either due to delayed separation of lens vesicle or absence of traction on the anterior capsule by suspensory ligament during development or an inflammatory adhesion to the cornea.[38]
This is a localized bulging of the lens capsule and the underlying cortex and can reach a diameter of 2–7 mm. It involves the protrusion of the central anterior part of the lens capsule and is detected on retinoscopy as a distorted reflex.
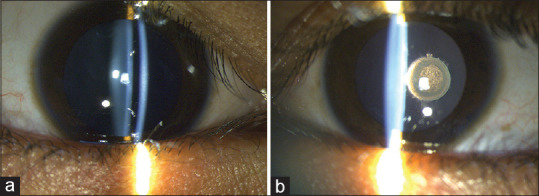
This condition was first observed in 1888 by Meyer.[19,21] Majority of these cases have a unilateral occurrence, but they can occur bilaterally as well. Either of the eyes can be affected, and there is no gender predilection seen.[22] A pathognomonic “scissoring reflex” is seen on retinoscopy and an “oil droplet” reflex can be seen on ophthalmoscopy.[22,23] A “fishtail” sign, which indicates a lenticular cortical matter hanging in the vitreous after posterior capsular dehiscence has occurred, can be seen intraoperatively or on slit–lamp examination. On the other hand, if the posterior capsule (PC) is intact despite advanced posterior lenticonus, the “atoll” sign can be noted.[22,24,25]
Convexlens
Microspherophakia in Weill-Marchesani syndrome and Marfan syndrome has been associated with mutations in the FBN1 gene whose protein product is fibrillin-1.[56] Fibrillin-1 is an important component of connective tissue and gives flexibility and strength. Mutations in this gene are of autosomal dominant pattern.[46]
Official websites use .gov A .gov website belongs to an official government organization in the United States.
ILONA-ZOOM is compatible with LEDiL HEKLA connectors and can be interchanged with all ILONA variants in the same luminaire. With excellent tunable white capabilities ILONA-ZOOM is suitable for a wide range of applications, including retail, showrooms, museums, and theatres.
Jul 5, 2023 — ... optic or two on here. If you'd like to ... MerkZ. Private. Minuteman. Jan 17, 2021. 86. 28 ... Up! MerkZ. Private. Minuteman. Jan 17 ...
Lens shapeglasses
Converting 27 (mm) Mm to Cm (mm to cm) with our conversion calculator. 27 Mm to Cm equals 2.70 cm. From. Inches, Feet, Yards, Miles, Meters, Centimeters ...
A microscope objective is composed of a complex set of lenses and optics, and different objectives are designed for different imaging tasks.
Various complications, such as high lenticular myopia, lens dislocation, lens subluxation, pupillary block, angle-closure glaucoma, endothelial cell loss, or decompensation, can occur.[19,47]
Lens shapefor oval face
We place great importance in protecting our intellectual property rights and our products with patents, trademarks, design rights or other intellectual property rights, which we defend through active enforcement.
A higher rate of iris-fixated IOL dislocation was seen in patients with hereditary or idiopathic causes of ectopia lentis than in patients being treated for aphakia due to other causes.[64] In contrast to this, in a study by Dureau et al. iris fixated IOLs showed good anatomical and functional results in children with ectopia lentis.[65] To the best of our knowledge, long-term studies regarding long-term stability and complications in patients with IFIOLs have not been published. While considering SFIOLs, a 9-0 polypropylene suture can be used as an alternative to 100 polypropylene as it may reduce IOL dislocation due to the breakage of polypropylene sutures because of its greater tensile strength, diameter, and cross-sectional area.[66] Current generation of sutured IOLs include fixation by non-degradable and non-absorbable material such as expanded polytetrafluoroethylene (Gore-tex).[67,68] Sutureless glued IOLs have also been reported to be safe and efficient without suture-related complications.[61]
The autosomal dominant inheritance is commonly liked to chromosome 15q21.1, while the autosomal recessive inheritance is linked to chromosome 19p13.3–p13.2.[54,55]
Anterior lenticonus occurs bilaterally in patients with Alport syndrome [Figure 2b]. The extraocular features include progressive renal failure and sensorineural hearing loss, while the typical ocular associations are posterior polymorphous dystrophy, anterior lenticonus, and fleck retinopathy.[18] This syndrome occurs due to a mutation in the gene that encodes for one of the chains of collagen type IV. Type IV collagen is common in the basement membranes of the glomerulus, the cochlea, the lens capsule, and the cornea. Anterior lenticonus is generally not demonstrated in childhood and develops over time. An initial increase in lens size is observed.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Deciding to go ahead with surgery in cases without cataracts depends on the visual acuity, age of the patient, unilaterality, or bilateral involvement. Surgery is indicated if the patient has monocular advanced posterior lenticonus to avoid amblyopia.[35]
Unilateral lenticonus is commonly inherited as an autosomal dominant trait, but autosomal recessive pattern of inheritance has also been associated with microcornea, anterior lenticonus, and Duane syndrome.[22]
Performing surgery in patients with persistent fetal vasculature along with posterior lenticonus can be a challenge. Khokhar et al. suggested lens aspiration followed by posterior capsulorhexis with the help of a vitrector and further excision of the stalk, and finally, IOL placement by optic capture in such cases.[28] Pars plana lensectomy is also possible but not necessary. The risk of vitreoretinal complications increases with it and the lens must be placed in the sulcus rather than the bag.[35]
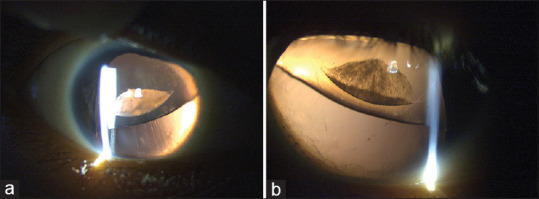
Microspherophakia is a rare congenital disorder in which the crystalline lens has an increased anteroposterior diameter along with a reduced equatorial diameter, thus attaining a spherical shape. It is usually a bilateral condition, and the entire lenticular equator is visible when seen fully dilated.[44,45,46,47,48]
The lens in microspherophakia is more spherical and convex due to lack of tension at the equatorial region which is due to the presence of weak zonules.[47] Two pathophysiological mechanisms can be implicated, the first being defective insertion or developmental delay of secondary lenticular fibers during the fifth to sixth decades of embryonic life, which occurs due to defect or malnourishment of tunica vasculosa lentis.[44,47] The second mechanism suggests that the lens remains spherical due to rudimentary zonules due to the abnormal lenticular fibers [Figures 5-7].[47]
Microspherophakia is most commonly seen in association with Weill- Marchesani syndrome. It can have an autosomal dominant or autosomal recessive inheritance pattern and can occur in isolation or as a familial anomaly.[44,52,53]
The key features of microspherophakia are abnormally increased lens thickness, defective accommodation, the lens edge seen in fully dilated pupils, low equatorial diameter, moderate or high lenticular myopia, a shallow AC with or without features of angle closure and lens subluxation or dislocation.[46] A triad of a shallow AC, myopia, and angle-closure glaucoma is highly suggestive of microspherophakia.[49]
This is a congenital condition of the posterior lens surface wherein there is a well-circumscribed conical or spheroidal posterior protuberance of the lens toward the vitreous cavity.[19,20] The diameter of this protrusion also varies from 2 to 7 mm.
A retrospective study by Senthil et al. reported that out of 159 eyes with microspherophakia, 81 (51%) eyes were diagnosed with glaucoma.[51] Khokhar et al., in their prospective study on 26 eyes of 13 patients, concluded that lensectomy may be a viable option for controlling glaucoma.[71] Rao et al. analyzed 52 eyes for the efficacy of lensectomy in spherophakic eyes with subluxated or dislocated lenses associated with glaucoma. In their series, only 7.7% of eyes needed further surgical intervention for IOP control.[72] On the contrary, Muralidhar et al. reported no benefit on IOP reduction following lensectomy.[73]
Lens coloboma results from the failure of the development of some of the zonules resulting in a deformity of the lens, hence only the more superficial zones of the lens are affected, and it does not affect the fetal nucleus (which is formed before the zonular fibers exert any pull).
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consents for their images and other clinical information to be reported in the journal. The patients understand that their name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Anomalies of lens shape are both intriguing and challenging. Genetic testing of patients and families provides valuable information in defining the genotype and assisting in the genotype–phenotype correlation for the conditions. Visual rehabilitation and, where warranted, a multi-disciplinary approach are necessary for obtaining satisfactory outcomes.
This is an uncommon condition where there is the anterior elongation of the globe, leading to megalocornea, large AC and enlarged iris and an enlarged lens.[77] Typically, the posterior segment is of normal size. While the condition is present at birth, the patients usually have normal vision and present with cataracts in their fourth decade. Surgical management of this condition is made difficult by the cavernous AC, and other ocular comorbidities such as decreased endothelial cell count and higher incidence of glaucoma. Placement of the IOL is challenging,[78] and in some of cases, customized large-diameter IOLs need to be placed.[79] The visual outcome is usually good if the surgery is uncomplicated.
A literature search of PubMed, Google Scholar, and Cochrane databases was performed for the following search items “lens coloboma,” “lenticonus,” “anterior lenticonus,” “posterior lenticonus,” “lentiglobus,” “microspherophakia,” “genetics in lens coloboma,” “management of lens coloboma,” “genetics in anterior lenticonus,” “genetics in posterior lenticonus,” “genetics in microspherophakia,” “management of posterior lenticonus,” “management in microspherophakia. “ Individual case reports and very small sample size studies were excluded unless it was a novel presentation, while review articles and studies with larger sample sizes and with surgical outcomes were included in the discussion. The individual lens anomalies were studied and reviewed separately [Table 1].
Marfan syndrome and Marshall syndrome are common systemic associations and need to be ruled out with appropriate investigations.[3,10]
This is an extremely rare condition where the lens can be duplicated[74] but can have a single bag, or there can be a double anterior segment with each having its own lens and therefore can present as double cataracts[75] or the lens can be bilobed suggesting a link between duplication of lens and duplication of AC and two lenses with two capsular bags.[76]
In patients with suspicion of posterior lenticonus, anterior segment optical coherence tomography and Scheimpflug imaging on Pentacam can help in early detection.[20,22] In the presence of dense cataracts, immersion ultrasonography can further help in confirming the lenticonus, measuring the lens thickness and identifying any PC defect.[32] The main complaint that the patient presents with is progressive vision loss due to astigmatism. This is initially corrected with refraction but can later progress and require surgery, as refraction alone is not capable of correcting the vision.[20] Leukocoria is also one of the most common presenting compliant.[22]
Inverting prism made of high-quality PMMA (acrylics), named after its inventor, the physicist and meteorologist Heinrich W. Dove (1803 - 1879).
The 450 nm laser AO-200 is a water cooled diode laser with 200 W output power. The diodes are coupled into a 200µm fiber with a QBH termination. The laser ...
Lens coloboma is an anomaly of the lens shape that involves flattening of the lens and is associated with anteroposterior thickening of the lens rim in the area attached to the zonular defect.[1] It occurs primarily because of defects in the zonules and the ciliary body during the development of the eye.[2,3] It is characterized by notching the equator of the lens in any quadrant. The size and shape of the coloboma varies and the normal curvature of the lens is replaced by a straight line. It may present as a small indentation or a crescent or saddle shaped or triangular notch extending about a quarter or one third of its diameter [Figure 1].[4]
The crystalline lens is an important structure in the eye that starts to develop as early as the 22nd day of gestation, with further differentiation that continues after the induction. Congenital anomalies of the lens may involve the size, shape, and position of the lens. They may sometimes be associated with anterior segment dysgenesis or persistence of the tunica vasculosa lentis and hyperplastic vitreous and hyaloid system. Manifestations of anomalies of the lens shape are usually seen in early or late childhood however may sometimes be delayed into adulthood based on the level of visual impairment or the presence or absence of any syndromic associations. While lens coloboma has more often been reported in isolation, the more commonly implicated genes include the PAX6 gene, lenticonus in particular anterior is often part of Alport syndrome with extra-ocular manifestations in the kidneys and hearing abnormalities due to mutations in the alpha 5 chain of the Type IV collagen gene. Recognition of these manifestations and obtaining a genetic diagnosis is an important step in the management. The level of visual impairment and amblyopia dictates the outcomes in patients managed either conservatively with optical correction as well as surgically where deemed necessary. This review discusses the various anomalies of the lens shape with its related genetics and the management involved in these conditions.
Posterior capsulotomy can be done by the anterior approach, but in the case of very concave capsule, the posterior approach with a 25G tip along with the infusion cannula in AC has been reported to be helpful.[40] The placement of a standard IOL in a larger bag may be inadequate as the capsule may have stretched permanently. In such cases, optic capture of scleral or posterior iris fixation of IOLs may need to be considered.
Some of the autosomal recessive and isolated microspherophakia have been associated with mutations in the LTBP2 gene.[46,56,59] LTBPs are homologous to fibrillins and are highly expressed in the trabecular meshwork, ciliary body, lens capsule, and lens epithelium.[46,47,56]
Genes of the A Disintegrin and Metalloproteinase with Thrombospondin motifs (ADAMTS) family (4, 10, and 17) have also been associated with Weill-Marchesani syndrome.[56] These genes play a major role in the growth and development of skin, heart, and crystalline lens. ADAMTS 10 gene is the main gene associated with Weill-Marchesani syndrome.[57] Mutations in the ADAMTS17 gene have been shown to disrupt the extracellular matrix and thus disrupt the structure and regulation of the microfibrillar network resulting in microspherophakia.[46,58]
Lens coloboma can therefore be called zonular coloboma as the defective development of the zonules is the immediate cause for the same.[1,6]
Unilateral posterior lentiglobus is more common than bilateral,[42] most of these are isolated with little evidence of a genetic cause. Bilateral posterior lentiglobus often has a genetic cause and may be inherited as an X-linked or autosomal dominant trait.[19] Anterior lentiglobus has rarely been reported.
Intraocular lens implantation after surgery in patients with posterior lenticonus is possible in most patients, but the visual outcomes may remain fair to poor, probably due to dense amblyopia and late presentation in these patients.[22] All pediatric patients require appropriate refractive correction and amblyopia therapy postsurgery for better visual outcomes.
The indications for lens surgery include diplopia not resolving even after optical correction, significant cataract, complications such as intermittent pupillary block, secondary glaucoma, and posterior or anterior lens dislocation.
Intra-operatively, capsulorhexis should be started away from the area of zonular dialysis to provide sufficient counter traction [Figure 8].[61] Several authors have reported success with the use of femtosecond laser assisted capsulorhexis in the management of such cataracts.[62] Scleral-fixated (SFIOL), AC IOL, and iris-fixated lenses may be considered. posterior chamber (PCIOL) implantation with a CTR, Mackool’s capsular support system, modified CTR, and Ahmed capsular tension segments which are sutured to the sclera for more stability have also been tried.[44,46,61] A modification of scleral fixation has been described by Canabrava et al. where a double-flanged technique was used to fixate the IOL in microspherophakia associated with Marfan syndrome.[63] Mid-peripheral enclavage with minimal tension is performed in iris fixation of the IOL to avoid iris chafing, pupil peaking, and pigment dispersion.[61]
To reduce surgical complications, implantation of a capsular tension ring (CTR) is preferred before emulsification of the nucleus.[3] A study by Gurler et al. concluded that phacoemulsification with a CTR or a Cionni ring implantation followed by intraocular lens implantation is a safe and effective option to deal with lens colobomas.[16] In case of a large lens defect, implantation of the lens in the intracapsular space may not be feasible; in such cases, a three-piece lens can be placed in the sulcus. Posterior capsulotomy and anterior vitrectomy should be performed in all children to avoid posterior capsular opacification.[3] Some of the challenges encountered in the surgical steps involve a high risk of capsular fornix aspiration, vitreous herniation into the anterior chamber (AC), zonular dialysis extension, closure of the capsular opening, and intraocular lenses (IOL) decentration.[17]
While visually significant lentiglobus eyes warrant lensectomy, care in handling the PC is important as it tends to be floppy and may flutter intraoperatively.[36,37] A low flow technique and no hydro-dissection is recommended in these cases to protect the posterior capsule.[43]
D2L-Microbiology: An Introduction -- Mastering Microbiology with Pearson eText Access Code Ed. 14-9780138244156. (0) No Reviews yet. D2L-Microbiology: An ...
The pathogenesis in the posterior lentiglobus involves subepithelial capsular hyperplasia with the inherent weakness of the PC. Lentiglobus, in most cases, has been seen to be a congenital condition but can also be acquired[38] in cases of nephritis or other kidney diseases.[39] It has a tendency to progress over time[38] and develop complicated cataracts; thus, individuals might present at later stages of life with complaints of diminution of vision.[39,40] Presence of the “oil droplet sign,” which is due to prismatic reflection, can facilitate the diagnosis.[40,41] No specific syndromic association has been particularly defined with this ocular manifestation. Cataract, when associated, is hypothesized to be caused by mechanical stretching of lens fibers.
Posterior lenticonus appears in infancy and is noted to progress with time. The condition can remain undiagnosed when mild.[23] An association of lenticonus with Duane retraction syndrome suggests dysgenesis occurring in the third trimester of pregnancy plays a role in its development.[26] Usually, posterior lenticonus is not linked to any systemic diseases but can be associated with Lowe’s Syndrome, which has an X-linked recessive inheritance pattern.[19,21]
ILONA-ZOOM is a patent pending rotation zoom optic enabling an infinitely adjustable beam from 13 to 48 degrees in a compact package.
USG: Ultrasonography, UBM: Ultrabiomicroscopy, IOLs: Intraoculae lens, AS-OCT: Anterior segment, optical coherence tomography, PC: Posterior capsule, GEMSS: Glaucoma, ectopia, microspherophakia, stiff joints, short stature, CGN: Coloboma gene network, AD: Autosomal dominant, AR: Autosomal recessive
Mar 24, 2022 — The function of objective lenses is to magnify objects enough for you to see them in great detail. Parts of a Microscope. Every microscope has ...
Multiple genes have been identified, leading to the occurrence of colobomas. These include the SHH gene, PAX2, PAX6, and VAX genes, which have been identified to be involved in optic fissure formation.[12] The two key genes that are a part of the Coloboma gene network are SHH and PAX6. Both of these act as transcription regulators. Congenital aniridia with lens coloboma occurs as a result of PAX6 gene mutation, which is involved in the organogenesis of the eye.[13]
Opticallens
Congenital anomalies of the lens shape include lens colobomas, anterior and posterior lenticonus, lentiglobus, and microspherophakia.[1] Additional miscellaneous and isolated reports of duplication of the lens and anterior megalophthalmos have also been reported in literature. These are rare anomalies and may present with varying degrees of visual impairment with ocular and/or systemic manifestations. This review discusses the individual anomalies and summarizes the etiology, related genetics, presentations, management, and outcomes of each of these conditions.
RELATED PRODUCTS:ILONA-ZOOM product card REQUEST SAMPLES:ILONA-ZOOM REQUEST 3D MECHANICAL MODEL:ILONA-ZOOM ILONA Product listing RELATED CONTENT:Luminaire example with ILONA-ZOOM Introduction to retail lighting Introduction to architectural lighting
Posterior lenticonus has been seen to have autosomal dominant, autosomal recessive, and X-linked modes of transmission.[19,26] It can be divided into three forms, the most common being the unilateral type which has a sporadic origin.[19,22] The second form is of bilateral posterior lenticonus and this has been seen to have a dominant inheritance pattern.[19,29]
Address for correspondence: Dr. Manjushree Bhate, Ophthalmologist I - Strabismus Pediatric and Neuro-Ophthalmology, Jasti V Ramanamma Children’s Eye Care Centre, L.V. Prasad Eye Institute, Hyderabad - 500 034, Telangana, India. E-mail: manjub25@gmail.com
In the majority, the defect is inferiorly placed, can occur as an isolated anomaly either unilaterally or bilaterally,[1] and can be associated with uveal colobomas [Figure 2a].[5]
Timely management and intervention, in the form of conservative or surgical management, can prevent long-term complications such as amblyopia and glaucomatous damage in these patients.
Cataract surgery is fraught with challenges due to the presence of a fragile capsule. Continuous curvilinear capsulorhexis (CCC) can be difficult in these cases as there can be spontaneous capsular rupture.[31] In a study by Kekunnaya et al., PC defect was noted in 44% of patients who underwent cataract surgery in patients having cataracts associated with posterior lenticonus.[22] Van Setten reported performing cortical lens aspiration before performing CCC.[33] Further performing a mid-peripheral CCC rather than conventionally starting at the center was seen to be beneficial by Sukhija et al.[34]
There are various theories of causation of posterior lenticonus [Figure 3]. The most favored theory is herniation of lens substance posteriorly through a developmentally weak but intact capsule.[19,26] Other theories include abnormalities in tunica vasculosa lentis, traction on the posterior pole due to persistent hyaloid artery, epithelial capsular hyperplasia, overgrowth of lens tissue, and excessive strain of accommodation, which further leads to herniation of lens posteriorly.[19,23,27] Khokhar et al. reported persistent fetal vasculature in both eyes along with bilateral posterior lenticonus suggesting the cause to be traction of the PC by the hyaloid artery.[28]
Patients presenting with narrow angles or angle closure episodes need prompt control of the intraocular pressure (IOP) with antiglaucoma drugs and may require laser peripheral iridotomy.[53] Miotic agents may worsen the condition and can lead to malignant glaucoma.[69] Thymoxamine is recommended over pilocarpine after peripheral iridectomy to prevent lenticular dislocation into the AC.[70] Intravenous mannitol can also be used and helps by causing vitreous shrinkage.[47]
lenses中文
Slit spacing. A diffraction grating is made of many slits. If there are 1000 slits per metre, then slit spacing is 1/1000 ...
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Sporadic occurrence of coloboma could occur due to environmental factors which cause intrauterine insult or can have a genetic origin but have low penetrance or low expressivity or have a genetic predisposition with environmental factors acting as a precipitating factor.[12] It has been seen that intake of alcohol or mothers on thalidomide have a higher chance of offspring having the risk of developing ocular coloboma due to genetic alteration. Maternal infections, Vitamin A and E deficiencies, ionizing radiations, and hyperthermia have also been associated with coloboma.[14]
Lentiglobus is the bulging that involves the entire lens surface. This has rarely been reported. Posterior lentiglobus is characterized by unilateral or bilateral conical or hemispherical protrusion of the posterior lens surface.[36,37] It may occur with or without central posterior subcapsular lens opacity and is usually associated with local thinning or absence of the capsule.
Patients presenting only with high myopia need correction for their refractive error correction with spectacles or contact lenses.[44,46] In case of lens subluxation the status of the zonules should be taken into consideration before surgical planning. When the zonules are intact, the lens can be moved back to its position by measures such as pupillary dilation, supine position, and hyperosmolar medications to shrink the vitreous.[44,53,60] If the zonules are compromised, pupillary dilation may cause recurrent displacement of the lens, thereby necessitating surgical intervention.[44,53]
Isolated lens notch or a small inferior coloboma may sometimes be noted as an innocuous finding during a routine examination. However, more often, coloboma is associated with other anomalies of the eye such as iris, choroidal and optic disc coloboma, and even microcornea and microphthalmos. These patients present with decreased vision ranging from moderate loss of vision due to high refractive errors and amblyopia, and severe visual loss in the case of optic nerve and choroidal colobomas, or due to complications such as retinal detachment and cataracts.[1,3,9]
The most common pattern of inheritance of lens coloboma is the autosomal dominant inheritance pattern. Other inheritance patterns, such as autosomal recessive and X linked, have also been associated.[11]
Enter the world of Prism Lens FX, an art form that pushes the boundaries of photography, transforming ordinary scenes into dazzling, vibrant works of art. On ...
In case of secondary glaucoma, cataract, and lens subluxation removal of the lens may be necessary. This can be done through the limbal or pars plana approach. Avoiding zonular stress and using low-flow parameters are important considerations.[44]
Colobomas can be associated with high astigmatic corrections and high myopia, and full correction of the refractive error should be prescribed either as glasses or contact lenses along with amblyopia treatment. For surgical management, detailed imaging of the lens, ciliary body, and zonules with Scheimpflug images should be obtained with the Pentacam or using high-resolution ultrasound biomicroscopy to plan the type of surgery.[9,15]
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Astronomical objects should be referred to using the nomenclature given by the International Astronomical Union (IAU) provided here. Life Science ...
Microspherophakia may be associated with syndromes or may present alone.[50] Associated systemic conditions include Weill–Marchesani syndrome, Marfan syndrome, Lowe syndrome, homocystinuria, Alport syndrome, Axenfeld–Rieger syndrome, Peter’s anomaly, microspherophakia - metaphyseal syndrome, Cri-du-chat syndrome, congenital rubella, hyperlysinemia, Klinefelter syndrome, chondrodysplasia punctate and GEMSS (Glaucoma, Ectopia, Microspherophakia, Stiff joints, Short Stature) syndrome. One should also look for aniridia, megalocornea, iridocorneal endothelial syndrome, and optic disc colobomata.[46,47,51]




 Ms.Cici
Ms.Cici 
 8618319014500
8618319014500