A rectangular prism of volume 84 cm3 has a mass of 760 g. ... - density of a rectangular prism
The basic biological mechanism behind the effects of LLLT is thought to involve the absorption of red and near-infrared light by mitochondrial chromophores, in particular cytochrome c oxidase (CCO), a component of the mitochondrial respiratory chain15,16,17. CCO activation results in increased production of adenosine triphosphate (ATP), which provides both the energy and phosphate required to regulate a variety of cellular functions. Consistent with this notion, the addition of exogenous ATP stimulated wound healing in an animal model18. Although wound contraction did not increase in mice treated with external ATP, in vitro observations suggest that ATP increases wound contraction by serving as an energy source for motility and contractile force generation, and as a phosphate donor for kinases regulating contraction19,20.
Depth of focus can have two slightly different meanings. The first is the distance over which the image plane can be displaced while a single object plane remains in acceptably sharp focus;[1][2][clarify] the second is the image-side conjugate of depth of field.[2][clarify] With the first meaning, the depth of focus is symmetrical about the image plane; with the second, the depth of focus is slightly greater on the far side of the image plane.
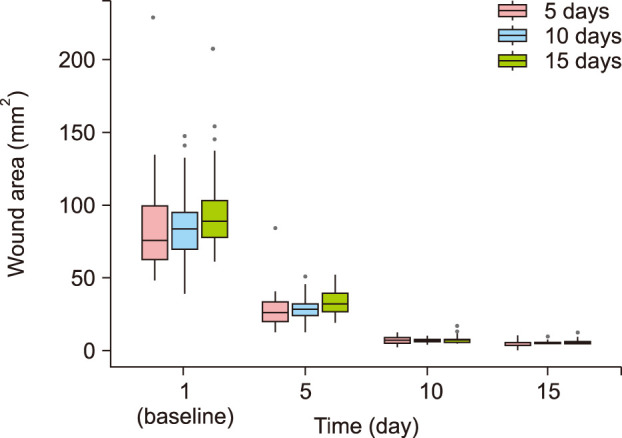
Values are presented as mean (standard deviation). NA: not applicable, IR5: 5 days of irradiation, IR10: 10 days of irradiation, IR15: 15 days of irradiation. *p-values are obtained by using ANOVA.
Regarding the wound healing of human skin, not only wound closure but also prevention of hypertrophic scars and keloids have great importance. In the context of formation of hypertrophic scar, the remodeling phase has critical role. Fibroblastic proliferation and excess collagen deposits are their two main characteristics, and imbalances in the rates of collagen biosynthesis and degradation, along with individual genetic predisposition, have been implicated in their pathogenesis21. It was recently proposed that poor regulation of interleukin (IL)-6 signaling and TGF β1 expression may play a significant role in this process22,23,24,25. LLLT can decrease IL-6 mRNA levels26, and has been proposed as an alternative therapy for hypertrophic scars. In three case studies, Barolet and Boucher27 reported significant improvements to scars after LLLT following scar revision by surgery or CO2 laser ablation. In fact, the mice in our study did not show any hypertrophic scar or keloid. Therefore, it is difficult to evaluate the effectiveness of LLLT for prevention of hypertrophic scar or keloid. Through previous studies that we mentioned above, however, more than 5 days of irradiation of LLLT might be helpful to prevent formation of hypertrophic scar or keloid. Further studies to evaluate the effectiveness of LLLT for prevention of human hypertrophic scars or keloids are needed.
Low-level laser (light) therapy (LLLT) is a promising technology used in various fields to stimulate healing, relieve pain and inflammation, and restore function to injured body parts. Since the initial experiments in 1983 studying the effects of low-level HeNe laser irradiation on wounds in rats, many studies have investigated wound healing by LLLT1.
The simple formula is often used as a guideline, as it is much easier to calculate, and in many cases, the difference from the exact formula is insignificant. Moreover, the simple formula will always err on the conservative side (i.e., depth of focus will always be greater than calculated).
FUNDING SOURCE: This work was supported by the GRRC program of Gyeonggi province [GRRC아주2016B04, Development of medical devices using LED]. The GRRC program of Gyeonggi province had no involvement in study design; collection, analysis and interpretation of data; and writing the manuscript.
The same factors that determine depth of field also determine depth of focus, but these factors can have different effects than they have in depth of field. Both depth of field and depth of focus increase with smaller apertures. For distant subjects (beyond macro range), depth of focus is relatively insensitive to focal length and subject distance, for a fixed f-number. In the macro region, depth of focus increases with longer focal length or closer subject distance, while depth of field decreases.
In astronomy, the depth of focus Δ f {\displaystyle \Delta f} is the amount of defocus that introduces a ± λ / 4 {\displaystyle \pm \lambda /4} wavefront error. It can be calculated as[4][5]
A few studies have directly compared the effects of different fluences of LLLT. Da Silva et al.6 investigated the effects of a 670 nm-wavelength laser on rats, by irradiating skin lesions with 0, 2, or 4 J/cm2 for 10 consecutive days. At 4 J/cm2, the re-epithelialization process was significantly faster than that in the other groups. A study using a 632.8 nm-wavelength laser reported that 3∼6 J/cm2 photostimulation facilitates the tissue repair process in diabetic wound healing by accelerating the rates of contraction and collagen production7. With irradiation at 830 nm, a preliminary investigation demonstrated that 5 J/cm2 LLLT improved wound healing, as measured by increased wound tensile strength8. A study in mice comparing the influences of 632.8, 785, and 830 nm lasers on burn wound healing found that treatment with 830 nm light at a fluence of 3 J/cm2 had profound effects on healing compared to untreated controls and mice treated with lasers of other wavelengths9. However, no studies have compared the effects of different fluences and irradiation durations on wound size reduction.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
In small-format cameras, the smaller circle of confusion limit yields a proportionately smaller depth of focus. In motion-picture cameras, different lens mount and camera gate combinations have exact flange focal distance measurements to which lenses are calibrated.
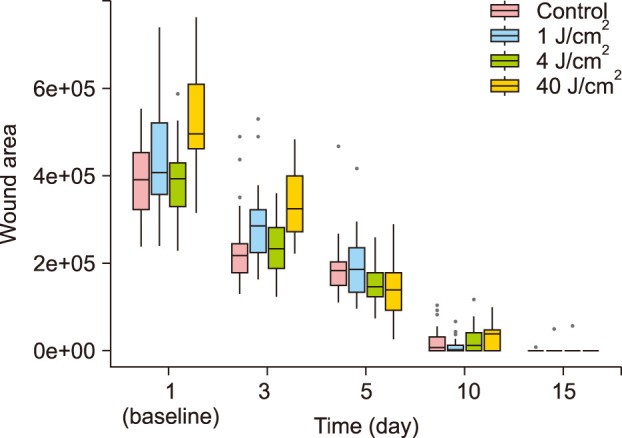
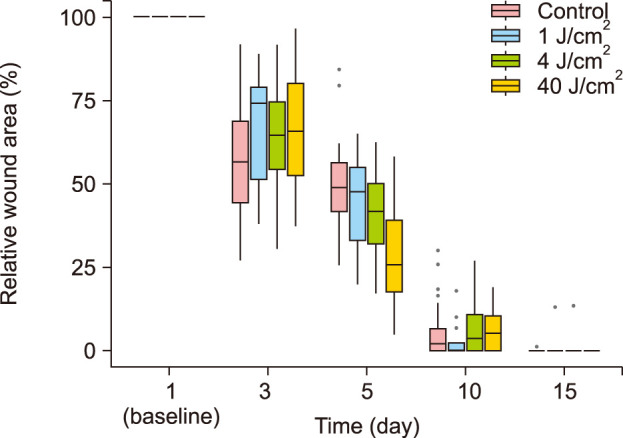
The most effective fluence level was 40 J/cm2 at day 5, as determined by monitoring wound closure. There were no statistically significant differences in wound healing with different durations.
Difference betweenlenses and depth of field
Corresponding author: You Chan Kim, Department of Dermatology, Ajou University School of Medicine, 164 World cup-ro, Yeongtong-gu, Suwon 16499, Korea. Tel: 82-31-219-5917, Fax: 82-31-216-9189, maychan@ajou.ac.kr
Shallowdepth of fieldphotography
After anesthesia by intraperitoneal injection of tiletamine/zolazepam (Virbac, Seoul, Korea) and xylazine (Bayer, Seoul, Korea) which was necessary to immobilize the mice, four full-thickness wounds were created on the dorsal skin of each mouse using a 8-mm-diameter punch. The wounds were left exposed without sutures or dressings. A total of 40 mice were used to compare the effects of different irradiation fluences on wound healing. The mice were divided randomly into untreated control (group A) and treated groups (n=10 per group). The wounds of the treated groups were irradiated at fluences of 1 J/cm2 (group B), 4 J/cm2 (group C), or 40 J/cm2 (group D) for five consecutive days starting on day 1 when the wounds were made. To determine the optimal duration of treatment, 30 mice (n=10 per group) were treated with 40 J/cm2 infrared light for 5 (IR5), 10 (IR10), or 15 (IR15) consecutive days. A low-intensity LED irradiation device named SHINeY (WON TECH Co., Seoul, Korea) was used as the light source. The intensity was 100 mW/cm2 and the spot size was 4.77 mm×13.15 mm. The distance between the light source and the dorsal skin was approximately 3 cm. Nonirradiated (control) mice were maintained under similar conditions.
Lenses and depth of fieldexplained
On days 1, 5, 10, and 15, images of the wounds were acquired, and the wound areas were measured as the primary outcome using Image-Pro Plus 6.0 software (Media Cybernetics, Silver Spring, MD, USA). The wound size immediately after wound creation was designated the original wound area. The percentage of wound closure at each time point was calculated using the following formula and defined as the secondary outcome.
ANOVA was used to compare wound size reduction between treatment groups and the statistical analyses were performed using R software, version 3.5.2 (R Foundation for Statistical Computing, Vienna, Austria). p-values <0.05 were considered statistically significant. Summary data are expressed as the mean±standard deviation.
We have shown that repeated exposure to low levels of light significantly stimulates wound healing in mice and demonstrated more efficient wound closure with certain fluences of 830 nm irradiation.
†Data are p-values, which are obtained by using t-test and corrected using the Bonferroni adjustment, which are significant when <0.05.
The magnification depends on the focal length and the subject distance, and sometimes it can be difficult to estimate. When the magnification is small, the formula simplifies to
However, after day 5, we observed no statistically significant differences between the groups irradiated with different fluences. The wounds of all groups were almost closed at day 15. We also investigated the effects of treatment duration, and observed no statistically significant differences between the groups. Wound closure begins with an inflammatory phase and re-epithelialization, followed by the remodeling phase, which generally begins 5 to 7 days after injury. In a previous study, while healing curves generated for control mice demonstrated an initial decrease in wound size during days 1 to 4 after injury, the wounds of LLLT-treated mice started to contract immediately after illumination11. Therefore, 5 days of irradiation could be adequate to reduce the wound area.
In conclusion, we have shown that repeated exposure to low levels of light significantly stimulates wound healing in mice and demonstrated more efficient wound closure with certain fluences of 830-nm irradiation. Conversely, the duration of irradiation did not significantly affect wound healing. Further studies regarding human wound healing will be required to examine the applicability of these results to clinical LLLT.
Depth of fieldmicroscope
Low-level lasers can affect lymphocytes, increasing their proliferation and activation; macrophages, increasing their phagocytosis; and fibroblasts, increasing their growth factor secretion and enhancing the uptake of both fibrin and collagen2. In addition, LLLT increases the motility of epithelial cells and the amount of granulation tissue produced during healing, and may reduce the synthesis of inflammatory mediators3,4, resulting in reductions in skin wound area in both humans and animals. However, the optimal physical variables for LLLT still lack consensus5.
In this study, we describe the effects of LLLT on wound size reduction in a standardized model of full-thickness excisional wound healing in mice, using an 830-nm diode laser with various fluence levels and durations of irradiation.
Low-level laser (light) therapy is a promising technology that stimulates healing, relieves pain and inflammation, and restores function in injured body parts. However, few studies have compared the effects of light-emitting diodes of different fluence levels or different treatment durations.
Wound closure involves the migration of the boundaries of an injury towards its center and can be assessed through related parameters, such as the percentage of wound contraction10. In this study, we investigated the effect of LED irradiation fluence on wound closure and the effect of the duration of LED irradiation on wound closure. Regarding the results of day 5, the most potent fluence was 40 J/cm2. Demidova-Rice et al.11 evaluated the effects of laser therapy on excisional wounds and found that the dose effects are not linear for various fluences of 635-nm light, with a maximum positive effect at 2 J/cm2. They reported that intensities of 1 and 10 J/cm2 improved healing to a lesser extent, while 50 J/cm2 had a negative effect on wound healing. Using 670-nm laser therapy, treatment at 4 J/cm2 displayed superior wound healing than treatment at 8 J/cm2.12 Inadequate doses can result in weak and insignificant effects; while excessive doses can cause negative or minimal effects13. With even higher doses, a biosuppressive or inhibitory effect may be observed14. In contrast to these studies, we used 830-nm light and observed an optimal fluence of 40 J/cm2. As light at this wavelength can penetrate the skin more deeply, we hypothesize that a higher fluence of irradiation might be required for wound healing at 830 nm. Further study is needed to investigate whether over 40 J/cm2 of fluence of irradiation has harmful effect on wound healing.
Depth of fieldphotography examples
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Depth of focus is a lens optics concept that measures the tolerance of placement of the image plane (the film plane in a camera) in relation to the lens. In a camera, depth of focus indicates the tolerance of the film's displacement within the camera and is therefore sometimes referred to as "lens-to-film tolerance".
Shallowdepth of field
While depth of field is generally measured in macroscopic units such as meters and feet, depth of focus is typically measured in microscopic units such as fractions of a millimeter or thousandths of an inch. In optometry depth of focus is usually measured in dioptres.
Following historical convention, the circle of confusion is sometimes taken as the lens focal length divided by 1000 (with the result in same units as the focal length);[2][3] this formula makes most sense in the case of normal lens (as opposed to wide-angle or telephoto), where the focal length is a representation of the format size. This practice is now deprecated; it is more common to base the circle of confusion on the format size (for example, the diagonal divided by 1000 or 1500).[3]
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Lenses and depth of fieldpdf
Lenses and depth of fieldcalculator
Eight-week-old female albino hairless mice (Skh:hr-1) weighing 25∼30 g were maintained in individual ventilated cage systems. The animals were group-housed, ten mice per cage. Constant temperature, humidity, and a 12-hour light/dark cycle were maintained, and the mice were fed a standard diet. All experimental protocols were approved by the Committee for Animal Care and Use of Ajou University (approval no. 2017-0016).
where t is the total depth of focus, N is the lens f-number, c is the circle of confusion, v is the image distance, and f is the lens focal length. In most cases, the image distance (not to be confused with subject distance) is not easily determined; the depth of focus can also be given in terms of magnification m:
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Full-thickness wounds were created on the dorsal skin using an 8-mm diameter punch, and the wounds were irradiated at 1, 4, or 40 J/cm2 for 5 consecutive days starting on day 1. To determine the optimal irradiation duration, wounds were irradiated at the most potent fluence of previous study for 5, 10, or 15 days. Photographic documentation, skin biopsies, and wound measurements were performed to compare the effects of different treatment parameters.
The choice to place gels or other filters behind the lens becomes a much more critical decision when dealing with smaller formats. Placement of items behind the lens will alter the optics pathway, shifting the focal plane. Therefore, often this insertion must be done in concert with stopping down the lens in order to compensate enough to make any shift negligible given a greater depth of focus. It is often advised in 35 mm motion-picture filmmaking not to use filters behind the lens if the lens is wider than 25 mm.
The other goal of our study was to identify the best duration of LED irradiation for wound healing. The effects of 5, 10, and 15 days of radiation (groups IR5, IR10, and IR15, respectively) were compared. Compared to their baseline values, wound areas steadily decreased in all groups (p< 0.001; Fig. 3, 4, and Supplementary Fig. 1). The wound healing was significant at day 5. The wounds of all groups almost closed on day 15. There was no significant difference in wound area reduction between the IR5 and IR10 groups nor between the IR5 and IR15 groups (Table 2). Post hoc analysis revealed no significant difference among the groups.
Our first goal was to identify the optimal fluence of LED irradiation to reduce the time required for wound closure. There were some variations in the sizes of the initial wounds, due to the difficulty in creating wounds in the flexible skin of the mice. Therefore, the relative wound area was analyzed along with the absolute values. Compared to the baseline values for each group, the wound areas in all groups steadily decreased over time (Fig. 1, 2). The wounds of all groups almost closed on day 15. Therefore, to assess when the effects of irradiation on wound healing appear, the analysis of wound closure at day 3, 5, 10 and 15 was done. When comparing the relative wound area in group A (control) with irradiated groups (group B, C, and D) respectively, more efficient wound closure was observed in group D (40 J/cm2) on day 5 (Table 1). At the same time, there was no significant difference in wound healing between groups A and B (1 J/cm2), C (4 J/cm2) respectively. Additionally, post hoc analysis was done and compared groups to each other. The most efficient fluence on day 5 was 40 J/cm2 (group D), which demonstrated significantly improved wound healing compared to all the groups. After day 5, no significant difference was observed among groups.
The phrase depth of focus is sometimes erroneously used to refer to depth of field (DOF), which is the distance from the lens in acceptable focus, whereas the true meaning of depth of focus refers to the zone behind the lens wherein the film plane or sensor is placed to produce an in-focus image. Depth of field depends on the focus distance, while depth of focus does not.
Articles from Annals of Dermatology are provided here courtesy of Korean Dermatological Association and Korean Society for Investigative Dermatology
†Data are p-values, which are obtained by using t-test and corrected using the Bonferroni adjustment, which are significant when <0.05.




 Ms.Cici
Ms.Cici 
 8618319014500
8618319014500