4K HDR Short Throw Smart Portable LED Projector - led projektoren
Fiber Optic Dual Arm Light. from $695.00 ; Fiber Optic Replacement Bulb. from $36.00 ; Fiber Optic Ring Light. from $695.00 ; LED 72 Bulb Ring Light. from $189.99.
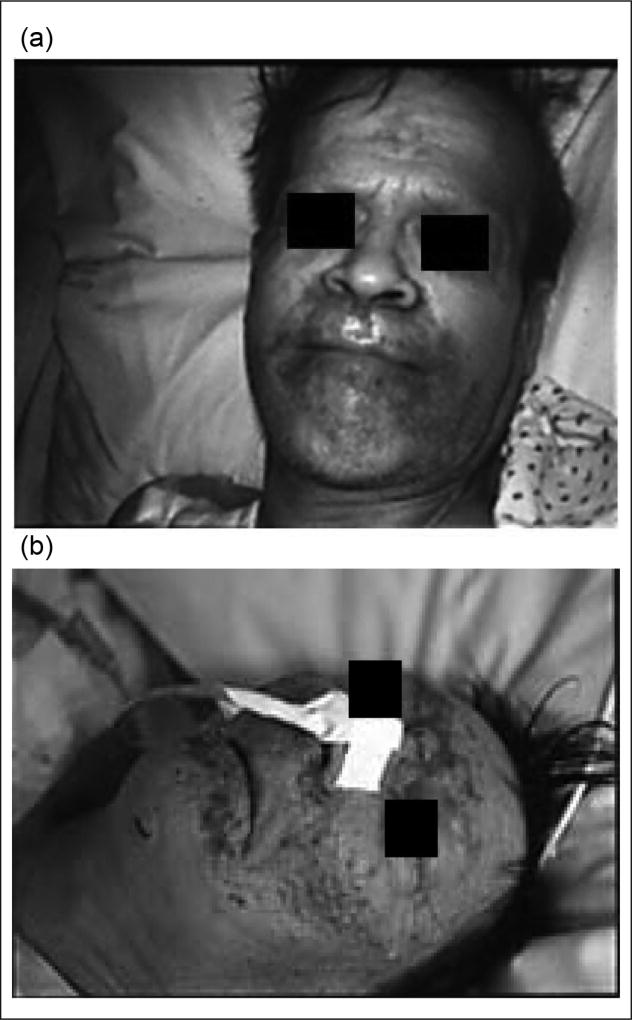
Patients with ALD and other forms of liver disease are predisposed to develop the skin lesions of zinc deficiency because of marginal underlying total body zinc stores. Several cases of acrodermatitis also have been reported in alcoholics with or without liver disease who were not receiving zinc in their hyperalimentation solutions or who had inadequate dietary intake of zinc (Figure 1).20–24
When white light enters the grating, the light components are diffracted at angles that are determined by the respective wavelengths (diffraction). Picking out ...
Portal systemic (hepatic) encephalopathy (PSE) is a derangement of mental function caused by liver disease or shunting of blood around the liver.29–31 This disordered mental state ranges in severity from intellectual impairment detectable only by careful psychometric testing to frank coma.29 Gut-derived toxins such as ammonia, mercaptans, short-chain fatty acids, false neurotransmitters, metabolites of tryptophan, and others are postulated to play an etiological role in this disordered mental status.29 Patients with cirrhosis have depressed serum zinc levels, and those with hepatic encephalopathy have statistically reduced serum zinc concentrations.32,33 Zinc is integrally involved in the metabolism of ammonia. Zinc deficiency markedly decreases activity of the urea cycle enzyme, ornithine transcarbamylase, and zinc supplementation corrects this.34 Similarly, zinc deficiency has been reported to impair activity of muscle glutamine synthetase, which causes hyperammonemia.35 Glutamine synthetase activity has also been reported to be decreased in patients with encephalopathy.36 Several trials have reported using zinc supplementation in various stages of PSE with somewhat inconsistent results. In the most recent large randomized clinical trial, polaprezinc supplementation plus standard therapy for 6 months (compared with standard therapy alone, protein-restricted diet with branched-chain amino acids and lactulose) was associated with a significant improvement in encephalopathy grade, blood ammonia levels, serum albumin levels, and a variety of psychomotor performance tests.37 Last, overt hepatic encephalopathy has been induced in a subject by creating zinc deficiency, and encephalopathy was then reversed with zinc supplementation.38
f/ftpcable
A long-term oral zinc supplementation (200 mg tid for 2–3 months) in cirrhotic patients, including alcoholics, produced beneficial effects on both liver metabolic function and nutrition parameters.103 Quantitative liver function tests, including galactose elimination capacity and antipyrine clearance, improved following oral zinc supplementation. Similarly, the Child-Pugh score, an overall clinical estimation of hepatocellular failure, was improved by zinc supplementation on average by greater than 1 point. Zinc supplementation also significantly improved nutrition parameters, such as serum prealbumin, retinol-binding protein, and insulin-like growth factor 1 (IGF-1). Indeed, the serum IGF-1 increased approximately 30% after zinc therapy. However, the nutrition parameters remained on average below the lower limit of the normal range.103 Studies evaluating specific mechanisms of action of zinc in ALD and long-term outcome studies are needed.
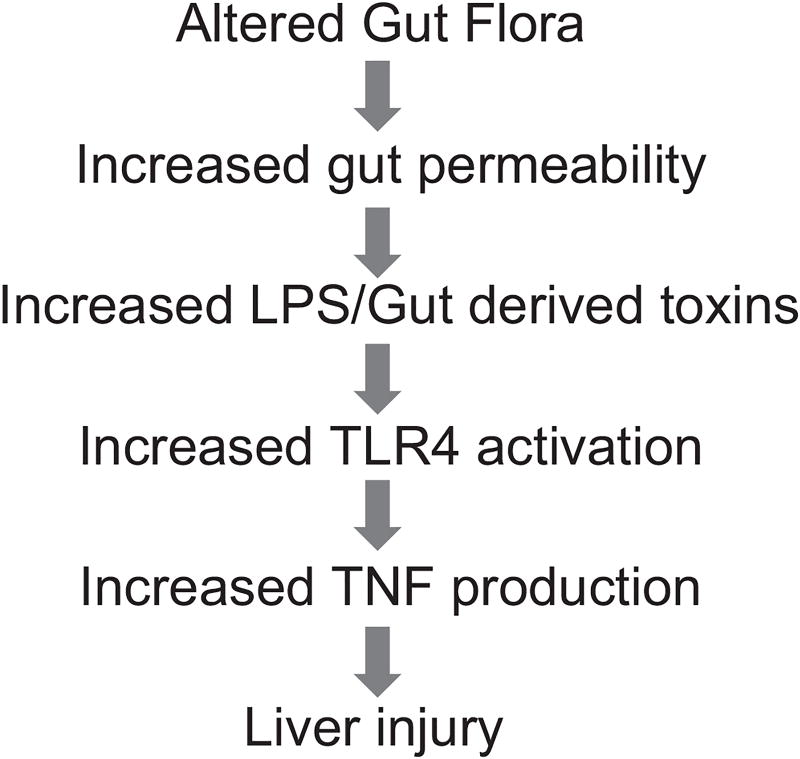
This graph depicts the gut-liver axis in alcoholic liver disease (ALD), beginning with altered gut flora and gut leakiness, leading to endotoxin-stimulated cytokine production, and, ultimately, liver injury and systemic inflammation. LPS, lipopolysaccharide; TLR, toll-like receptor; TNF, tumor necrosis factor.
The effects of zinc deficiency are particularly obvious on the skin, as manifested by an erythematous rash or scaly plaques. Many common dermatological conditions (eg, dandruff, acne, diaper rash) have been associated with zinc deficiency or effectively treated with zinc.15 Acrodermatitis enteropathica (AE) is a rare hereditary disease characterized by skin lesions, alopecia, failure to thrive, diarrhea, impaired immune function with frequent infections, and, in some cases, ocular abnormalities.16–19 The skin lesions (acrodermatitis) tend to occur around the eyes, nose, and mouth; over the buttocks and perianal regions; and sometimes in an acral distribution. The signs and symptoms of AE are caused by zinc deficiency due to impaired intestinal absorption of zinc. AE is caused by mutations of the SLC39A4 gene on the chromosome band 8q24.3, encoding a zinc transporter in humans (Zip4).19
STPcableused for
Zinc absorption, transfer, and excretion are accomplished by 2 large classes of transporters that tend to have opposing effects (ZnT proteins and Zip transporters).73,77–79 The Zip family of transporters move zinc from the extracellular space into the cellular cytoplasm. Indeed, Zip4 plays a major role in intestinal zinc absorption, and a lack of this transporter causes acrodermatitis enteropathica. The ZnT proteins generally work in opposition to the Zip transporters.
Early studies by Henkin et al28 reported that experimentally induced zinc deficiency in humans may be accompanied by apathy or irritability, which is reversed with zinc supplementation. Similarly, children with AE may have apathy or confusion, which responds to zinc supplementation. We have observed patients receiving parenteral nutrition (PN) who developed severe depression or confusion and severe hypozincemia. Marked improvement in mental status coincided with zinc supplementation in these patients.20,21
There have been multiple studies showing that zinc supplementation reverses known manifestations of zinc deficiency in ALD, such as impaired night vision, skin lesions, and, in some cases, encephalopathy and immune dysfunction.12 Studies have been performed to determine the duration and amounts of zinc necessary to improve serum and hepatic zinc in patients with ALD. Alcoholic patients without cirrhosis received zinc sulfate at 600 mg/d for 10 days and alcoholic cirrhotics for 10, 30, and 60 days.102 Serum zinc concentrations increased to normal values in all groups of patients during 10 days to 2 months of zinc supplementation. Zinc concentrations in the liver biopsies were significantly increased in patients with cirrhosis after zinc supplementation for 10 and 60 days, but some patients remained under normal values, particularly those with cirrhosis. No adverse reactions of zinc supplementation were observed in this short-term study.
s/ftpcablemeaning
As noted above, endotoxemia plays an important role in the development of ALD through stimulating proinflammatory cytokine production.83 Disruption of the intestinal barrier has been suggested to be a leading cause of alcohol-induced endotoxemia.83 Alcoholic patients showed increased gut permeability to a variety of permeability markers, such as polyethyleneglycol, mannitol/lactulose, or 51CrEDTA.91–94 In animal studies, gut permeability to macromolecules such as horseradish peroxidase (HRP) was increased in association with alcohol-induced plasma endotoxemia and liver damage.95–98 We showed that orally administrated LPS can be detected in the plasma of alcohol-intoxicated mice but not in control mice,99 providing direct evidence that alcohol increases gut permeability to endotoxin. Animal studies also showed that preventing gut leakiness results in suppression of alcohol-associated endotoxemia and liver damage, suggesting that gut leakiness is a causal factor in the development of alcoholic endotoxemia and liver injury.96,97,99
Zinc is an essential nutrient for a broad range of biological activities. In the United States, the Recommended Dietary Allowance (RDA) is 8 mg/d for women and 11 mg/d for men older than age 19. Red meats, especially beef, lamb, and liver, as well as certain sea foods (eg, oysters), have some of the highest concentrations of zinc in food. Zinc and dietary protein directly correlate with each other. Patients with liver disease, especially ALD, often have poor diets that are low in protein and low in zinc. Moreover, some dietary fibers/phytates can reduce zinc absorption. Absorption of zinc is concentration dependent and occurs throughout the small intestine (mainly the jejunum). Absorption may be impaired in cirrhosis, and typically there is increased urinary excretion of zinc in cirrhosis.12
Eyepieces. When microscopes were first invented, eyepieces played a major role in their design since they were the only means to actually see the object under ...
Hepatocyte regeneration after liver injury represents a form of wound healing. After partial hepatectomy or liver injury, hepatocytes undergo a synchronized, multistep process consisting of priming/initiation, proliferation, and termination. These steps are essential for restoring the structure and functions of the liver. The regenerating liver requires a large amount of zinc over a short period of time. This demand is met, in part, by induction of the zinc/copper binding protein metallothionein.67 Metallothionein can transfer zinc to various metalloenzymes and transcription factors, and metallothionein knockout mice have impaired liver regeneration.68 Thus, zinc is essential for wound healing at peripheral sites as well as for liver regeneration.
Because of the above-noted findings, we carried out a series of studies to determine whether zinc deficiency is related to the deleterious effects of alcohol on the intestinal barrier. We fed mice an alcohol or isocaloric liquid diet for 4 weeks, and liver injury was detected in association with elevated blood endotoxin level.100 Alcohol exposure significantly increased the permeability of the ileum. Reduction of tight-junction proteins in the ileal epithelium was observed in alcohol-fed mice. Alcohol exposure significantly reduced the ileal zinc concentration in association with accumulation of reactive oxygen species. Using in vitro studies, Caco-2 cell cultures demonstrated that alcohol exposure increased the intracellular free zinc because of oxidative stress. Zinc deprivation caused epithelial barrier disruption in association with disassembling of tight junction proteins in the Caco-2 monolayer cells.100 Furthermore, minor zinc deprivation exaggerated the deleterious effect of alcohol on the epithelial barrier.100 In summary, alcohol disrupts intestinal barrier function and induces endotoxemia, in part, by causing alterations in intestinal zinc homeostasis. Zinc supplementation partially protects against this increased permeability, endotoxemia, increased cytokine production, and subsequent liver injury.
The effect of zinc deficiency on immune function in humans was initially studied in children with AE.69 Leukocyte function and cell-mediated immunity were impaired in these children and corrected with zinc supplementation. Golden et al70 described thymic atrophy in children with protein energy malnutrition and zinc deficiency, and this thymic atrophy reversed with zinc supplementation. We reported 2 patients who developed severe zinc deficiency with acrodermatitis while on PN. These patients had cutaneous anergy and markedly depressed T cell response to phytohemaglutinin,71 which corrected with zinc supplementation alone.
Zinc deficiency is a well-recognized cause of hypogonadism in experimental animals and humans.56 Chronic alcoholics with and without liver disease and other patients with liver disease of multiple etiologies may have hypogonadism.57 The hypogonadism of zinc deficiency appears to be primarily a gonadal defect.56,58 Adequate levels of gonadotrophins and intact gonadotrophin response to luteinizing hormone–releasing hormone have been demonstrated in zinc-deficient animals. Zinc-deficient animals have reduced basal testosterone levels and depressed weights of testes and other androgensensitive organs compared with zinc-sufficient controls.58 Humans fed a zinc-deficient diet developed decreased libido, depressed serum testosterone levels, and marked reduction in sperm counts.59,60 Moreover, zinc supplementation significantly increased serum testosterone in elderly men with marginal zinc deficiency. Zinc is also required for maintenance of sperm cells, progression of spermatogenesis, and sperm motility.61,62
Impaired night vision has been recognized in alcoholic cirrhotics since the late 1930s, and this has been confirmed in recent studies in many types of cirrhosis.39–41 This is usually associated with vitamin A deficiency, and vitamin A supplementation improved night vision. Several groups, including our own, have shown that some individuals with cirrhosis require not only vitamin A but also zinc supplementation to correct or improve their dark adaptation.42,43 Zinc and vitamin A interact on many different levels, including production of retinol-binding protein and activity of retinol dehydrogenase. Studies in zinc-deficient experimental animals also demonstrated progressive anatomic deterioration of the retina.44,45 Similar retinal degeneration was observed in a patient with AE.46 Thus, there is strong clinical and experimental evidence that zinc affects retinal function, and zinc supplementation may improve dark adaptation in some patients with liver disease.
A major and initial manifestation of zinc deficiency is anorexia with subsequent weight loss.47 The mechanism(s) by which zinc deficiency produces anorexia is unknown. Initially, alterations in taste acuity and in circulating amino acids were implicated as etiologic factors.48,49 We showed that zinc deficiency in the rat affected catecholamine levels in total brain and in specific regions of the hypothalamus. We demonstrated that zinc-deficient animals are resistant to the central administration of known inducers of food intake such as norepinephrine and muscimol.50 Zinc is extremely important for normal membrane structure and function.51 We speculated that there is a decrease in receptor responsivity in the zinc-deficient animal, possibly secondary to alterations in membrane fluidity, which may explain, at least partially, the severe anorexia noted in these animals.
Liver disease, especially alcoholic liver disease (ALD), has been associated with hypozincemia and zinc deficiency for more than half a century.1,2 These early ALD observations were confirmed by multiple investigators, and tissue concentrations of zinc have been demonstrated to be decreased in alcoholic cirrhosis as well as animal models of liver disease.3–11 This article updates these early observations on dysregulated zinc metabolism in liver disease with new advances in this area and will review (1) clinical manifestations of zinc deficiency and their relevance to liver disease, (2) zinc metabolism, (3) zinc and ALD, (4) zinc and viral liver disease, (5) zinc and other liver diseases, and (6) general recommendations concerning zinc supplementation and overall conclusions.
Zinc can attenuate oxidative stress through introduction of metallothionein and through multiple other mechanisms, such as inhibiting TNF and modulating multiple enzymes. Zinc supplementation in a mouse model of ALD attenuated alcohol-induced liver injury as measured by histopathological and ultrastructural changes, serum alanine transferase activity, and hepatic TNF-α levels. Zinc supplementation inhibited accumulation of ROS as indicated by dihydroethidium fluorescence and the subsequent oxidative damage as assessed by immunohistochemical detection of 4-hydroxynonenal and nitrotyrosine and quantitative analysis of malondialdehyde and protein carbonyl in the liver.101 Zinc supplementation suppressed alcohol-elevated CYP 2E1 activity but increased the activity of alcohol dehydrogenase in the liver. Zinc supplementation also prevented alcohol-induced decreases in glutathione (GSH) concentration and glutathione peroxidase activity and increased glutathione reductase activity in the liver.8,101
FTPcablevs UTP
Applications10GBase-T ( IEEE 802.3an)1000Base-TX ( TIA/EIA-854)1000Base-T ( IEEE 802.3ab)100 Base-TX ( IEEE 802.3u)10base-T ( IEE 802.3)
This playlist covers the various topics of analog electronics and the related solved examples. The following topics are covered in this playlist.
Hepatitis B virus (HBV) is an even more serious public health problem, with more than 350 million infected people worldwide. Serum zinc levels are significantly decreased in patients with acute hepatitis B infection and are frequently depressed with HBV cirrhosis (similar to HCV cirrhosis).117,118 Specifically designed zinc finger proteins had been used in an attempt to inhibit HBV viral transcription with some success, and this is a potential therapeutic target for new HBV drugs.119 Importantly, marginal zinc deficiency appears to impair the efficacy of hepatitis B vaccination.120 This is another example of how zinc deficiency may impair immune function with special relevance to liver disease.
ALD continues to be a major cause of morbidity and mortality in the United States. Two-thirds of Americans consume alcohol, and an estimated 14 million Americans are alcoholics.80 It has been estimated that 15%–30% of heavy drinkers develop advanced ALD. Alcoholic cirrhosis accounts for more than 40% of all deaths from cirrhosis and for 30% of all hepatocellular carcinomas.80–82 Significant advances have been made in our understanding of the pathophysiologic mechanisms of ALD. However, there is still no Food and Drug Administration (FDA)–approved therapy for this common and often devastating disease. Interactions between the bowel, immune system, and the liver are critical components of ALD. In this model, chronic alcoholism results in changes to the intestinal epithelial barrier, leading to increased gut permeability.83 Subsequently, endotoxin or lipopolysaccharide (LPS), a component of the gram-negative bacterial cell wall, translocates across the disrupted intestinal barrier and enters the portal venous circulation to stimulate primed Kupffer cells. This results in both proinflammatory cytokine production and generation of reactive oxygen species, key mediators of ALD (Figure 3).81–83 Zinc deficiency is well documented in both humans with alcoholic cirrhosis and in animal models of ALD.8 In a representative human study, the serum zinc concentration in alcoholic patients was 7.52 µmol/L, which was significantly lower than 12.69 µmol/L in control subjects.84 Moreover, the decrease in serum zinc correlates with progression of liver damage. Patients with alcoholic cirrhosis had a lower serum zinc level (80 µg/dL) than noncirrhotic patients (97 µg/dL), decreased by –37% and –24%, respectively, compared with healthy individuals (127 µg/dL).85 We have demonstrated that zinc supplementation attenuates ethanol-induced liver injury in murine models.8,86–90 Importantly, zinc protected intestinal barrier function to prevent endotoxemia, reducing both proinflammatory cytokine production and oxidative stress (Figure 4). These data provide a strong rationale for zinc supplementation in human ALD. Below, we discuss in greater detail the effects of zinc deficiency/zinc supplementation on specific pathways for ALD.
Much of our knowledge concerning the metabolic functions of zinc in humans is derived from manifestations of zinc deficiency in zinc-deficient animals, in patients with acrodermatitis enteropathica (a hereditary disease of impaired zinc absorption), or in patients with acquired zinc deficiency due to an underlying disease process.12 It is also becoming clear that clinical and biochemical manifestations of zinc deficiency often occur when some stress is placed on the organism.13,14 In liver disease, this stress may occur through increased gut permeability with endotoxemia, infections such as spontaneous bacterial peritonitis, or release of stress hormones. Selected potential clinical manifestations of zinc deficiency in liver disease are shown in Table 1.
by JM Carmona · Cited by 60 — an infrared (IR) cutoff correlated to its UV one. However, using very plausible arguments [5], they noticed that conventional QFT should fail at an entropy ...
UTPcable
The role of zinc in nucleic acid metabolism, in the synthesis of structural proteins such as collagen, and in a host of enzymatic pathways makes zinc balance important for wound healing. A clinical role for zinc in wound healing was initially postulated by Pories et al63 with the observation of improved healing of pilonidal sinuses with zinc administration. Subsequent controlled studies by Hallböök and Lanner64 demonstrated that zinc supplementation improved wound healing in patients with both venous leg ulcers and decreased serum zinc concentrations. Several investigators then reported depressed wound healing in experimental animal models (eg, thermal and excised wounds, gastric ulcers) in zinc-deficient compared to zinc-sufficient animals.65,66 Recent studies have supported the important clinical role of zinc in wound healing, especially in leg ulcers.
Approximately 3% (~170 million) of the world’s population has been infected with HCV. For most countries, the prevalence of HCV infection is <3% (2% in United States).104,105 Approximately 70% of acute HCV infection progresses to chronic liver disease. The current standard of care for chronic HCV infection is based on the combination of pegylated interferon and ribavirin. Approximately 40%– 50% of genotype 1, by far the most frequent HCV genotype in the United States, is cured with this type of therapy. Specific protease inhibitors, telaprevir and boceprevir, became available in 2011, and this new addition to the interferon and ribavirin regimen should substantially increase the cure rate of both naive patients and many individuals who have already been treated.104,105
Patients with alcoholic liver disease frequently complain of anorexia and have decreased food consumption.52,53 Patients with acute liver disease also frequently complain of unpleasant olfactory and gustatory sensations, and this usually improves as the liver disease resolves. Burch et al54 reported decreased taste and smell acuity in cirrhotics with hypozincemia. Smith et al55 demonstrated objective disordered gustatory acuity in both viral hepatitis patients and patients with chronic liver disease (both groups had hypozincemia).
Zinc is the second most prevalent trace element in the body. It is integrally involved in the normal life cycle and has many important regulatory, catalytic, and defensive functions. Zinc was shown to be an essential trace nutrient for rodents in the 1930s and in humans in 1963, and it plays a catalytic role in a host of enzymes. Zinc plays a major role in the regulation of gene expression through metal-binding transcription factors and metal response elements in the promoter regions of the regulated genes. Zinc also plays a critical role in zinc-finger motifs. Zinc fingers typically have 4 cysteines within the protein that allow zinc to be bound in a tetrahedral complex.
u/ftpcablemeaning
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Similar to ALD, the serum levels of zinc are often decreased in HCV patients, and serum levels also tend to negatively correlate with hepatic reserve and to decrease with interferon-based therapy.105–108 Serum zinc levels are not only decreased in many patients with hepatitis C, but there are functional correlations with the reduced serum zinc levels. For example, patients have reduced taste sensitivity that correlates with their reduced serum zinc levels. Moreover, it is increasingly recognized that some patients with hepatitis C have decreased skin levels of zinc as well as serum zinc levels.106 HCV patients may present with necrolytic acral erythema, which responds to zinc supplementation (discussed above).
Zinc is an essential trace element required for normal cell growth, development, and differentiation. It is involved in DNA synthesis, RNA transcription, and cell division and activation. It is a critical component in many zinc protein/ enzymes, including critical zinc transcription factors. Zinc deficiency/altered metabolism is observed in many types of liver disease, including alcoholic liver disease (ALD) and viral liver disease. Some of the mechanisms for zinc deficiency/ altered metabolism include decreased dietary intake, increased urinary excretion, activation of certain zinc transporters, and induction of hepatic metallothionein. Zinc deficiency may manifest itself in many ways in liver disease, including skin lesions, poor wound healing/liver regeneration, altered mental status, or altered immune function. Zinc supplementation has been documented to block/attenuate experimental ALD through multiple processes, including stabilization of gut-barrier function, decreasing endotoxemia, decreasing proinflammatory cytokine production, decreasing oxidative stress, and attenuating apoptotic hepatocyte death. Clinical trials in human liver disease are limited in size and quality, but it is clear that zinc supplementation reverses clinical signs of zinc deficiency in patients with liver disease. Some studies suggest improvement in liver function in both ALD and hepatitis C following zinc supplementation, and 1 study suggested improved fibrosis markers in hepatitis C patients. The dose of zinc used for treatment of liver disease is usually 50 mg of elemental zinc taken with a meal to decrease the potential side effect of nausea.
202419 — These specifications tell you the optical performance, such as magnification, aberration correction, and other parameters.
Most forms of zinc salts have nausea and epigastric distress as potential side effects. Consuming zinc with a meal or switching types of supplements (eg, switch from zinc sulfate to zinc gluconate or acetate) may lessen these symptoms. We use a once-daily dose of 50 mg elemental zinc to not inhibit copper absorption. In Wilson disease, split doses (usually 50 mg of elemental zinc 3 times per day, separated from meals) are required to cause appropriate reduction in copper burden. Moreover, it appears that some patients may not be zinc responsive, and adherence to therapy and careful monitoring are absolutely critical.
Apoptosis is a major mechanism of hepatocyte death in ALD. We evaluated the possible beneficial effects of zinc therapy in experimental ALD. Adult male mice fed an alcohol liquid diet for 6 months developed hepatitis as indicated by neutrophil infiltration and elevation of the chemokines, keratinocyte chemoattractant, and monocyte chemoattractant protein-1. Apoptotic cell death was detected in alcohol-exposed mice by a terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assay and confirmed by the increased activities of caspase-3 and −8. Zinc supplementation attenuated alcoholic hepatitis and reduced the number of TUNEL-positive cells in association with inhibition of caspase activities.90 The mRNA levels of TNF-α, TNF-R1, FasL, Fas, FAF-1, and caspase-3 in the liver were upregulated by alcohol exposure and were attenuated by zinc supplementation.89,90 Zinc supplementation also prevented elevated serum and hepatic TNF-α levels and TNF-α R1 and Fas proteins in the liver associated with alcohol feeding. Thus, zinc supplementation attenuated the increase in factors known to be associated with hepatic apoptosis.8,90
FTPcablefull form
Zinc deficiency is also associated with necrolytic acral erythema (NAE).25 NAE is a recently recognized dermatosis, presenting in the form of pruritic, symmetric, well-demarcated, hyperkeratotic, erythematous-to-violaceous, lichenified plaques with a rim of dusky erythema on the dorsal aspects of the feet and extending to the toes. NAE is associated with decreased serum and skin zinc levels and is almost always associated with HCV infection, thereby serving as a cutaneous marker for underlying HCV infection.26 Use of oral zinc therapy is highly effective and leads to NAE resolution in combination with treatment of the underlying HCV infection.27
Correspondence Author: Craig J. McClain, University of Louisville Medical Center, 550 S Jackson St, ACB 3rd Floor, Louisville, KY 40292, USA, craig.mcclain@louisville.edu
Zinc status and the serum zinc level drop with low dietary zinc intake. There normally are multiple mechanisms in place to protect against zinc deficiency, including increased absorption and decreased excretion via modification of zinc transporters.77,79 Zinc status is typically assessed by plasma/serum zinc concentration. However, inflammation/stress hormones may cause a decrease in serum zinc level, with an internal redistribution of the zinc (Figure 2).13,14,79 This stress response is often associated with hypoalbuminemia. Albumin is a major binding protein for zinc, but the serum zinc concentration will decrease with an inflammatory stimulus even in the absence of hypoalbuminemia (Figure 2).13 This is mediated at least in part by changes in zinc transporters, especially induction of Zip14 and induction of hepatic metallothionein.73 Metallothionein is a metal-binding protein that serves many functions, including zinc transport, antioxidant activity, and modulation of zinc absorption.8,77,79 Indeed, ingestion of pharmacologic amounts of zinc causes induction of intestinal metallothionein, which then inhibits intestinal copper uptake and induces negative copper balance in the treatment of Wilson disease (discussed subsequently).
Several groups have reported decreased serum levels of zinc in HCC patients. In a case-control study comparing patients with HCC, cirrhosis, and benign digestive disease, serum levels of Zn in patients with HCC were significantly lower than in those patients with benign digestive disease and similar to levels in cirrhotic patients.131 Nakayama et al132 reported depressed levels of zinc in patients with chronic hepatitis and hepatocellular carcinoma compared to healthy volunteers. They also tested the metallothionein levels of these individuals and found that patients with cirrhosis and hepatocellular carcinoma had levels significantly lower than those in patients with chronic hepatitis and controls. When levels of zinc in HCC tumor tissue were studied, they were found to be significantly decreased compared to surrounding nontumor tissue, and levels in nontumor tissue were significantly lower than normal liver tissue.133–141 Kubo et al142 investigated metallothionein (MT) levels by high-performance liquid chromatography (HPLC) analysis in resected HCC tumors, surrounding noncancerous but diseased hepatic tissue, and normal liver tissue obtained from autopsies done on patients with no liver disease. They found that MT existed mainly as Zn-MT in normal hepatic tissue, whereas in the noncancerous parenchyma surrounding HCC, the Zn-MT was replaced to a significant extent by Cu,Zn-MT. In the cancerous tissue, the Cu,Zn-MT was largely displaced by Cu-MT, and Zn-MT was undetectable.
Healthy volunteers were injected intravenously with low-dose endotoxin or lipopolysaccharide (LPS). There was a marked reduction in the serum zinc level, which nearly normalized by 24 hours. A second dose of LPS caused a similar reduction in serum zinc. Injection of vehicle caused no significant reduction in zinc. Importantly, this very low dose of endotoxin caused no changes in the serum albumin.13 Thus, the hypozincemia was not secondary to a drop in the serum albumin level.
DescriptionCAT6A ( CAT6 Augmented ) cable is an ideal solution for 10G network. It supports the higher frequencies required for 10G Ethernet and fully backwards compatible with CAT6 and CAT5e. All of our CAT6A cables are double shielded and fully screened to ensure immunity from Alien Crosstalk and other external interference and are specified up to frequencies of 500Mhz.SSTP (Screened Shielded Twisted Pair) or SFTP (Screened Foiled Twisted Pair) cabling offer shielding between the pair sets and an overall sheath shield within the 100 Ohm twisted pair cable. This type of shielding protects EMI from entering or exiting the cable and also protects neighboring pairs from crosstalk. Standards
There are many therapeutic reasons why zinc may be beneficial in the treatment of hepatitis C, including (1) anti-oxidant function, (2) regulation of the imbalance between TH1 and TH2 cells, (3) zinc enhancement of antiviral effects of interferon, (4) inhibitory effects of zinc in the HCV replicon system, and (5) hepatoprotective effects of metallothionein.105,109 Several studies have evaluated the role of zinc as an adjunct therapy for eradication of the HCV. Initial studies indicated that administration of zinc in combination with interferon was more effective than interferon alone.110,111 However, in subsequent studies, when pegylated interferon and ribavirin were used in combination, the addition of zinc generally produced limited benefits on viral clearance.112 Some of these combination studies have shown improved transaminases or fewer medication side effects while on zinc therapy.113–115
Hepatocellular carcinoma (HCC) is the third leading cause of cancer mortality worldwide and the ninth leading cause of cancer deaths in the United States.127 Its incidence and mortality rates in the United States are increasing. The survival rate continues to be dismal with an overall 5-year survival of only 13%.128 The high mortality is due to late-stage detection of this cancer when most of the therapies available are not effective. Globally, 78% of HCC can be attributed to chronic HBV and chronic HCV viral infection.129 In United States, alcoholism is the most common cause of HCC.130
2024630 — The base of the microscope provides stability and support for the entire microscope, ensuring that it remains steady during observation.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Zinc deficiency can disrupt intestinal-barrier function in vitro (a), and zinc deficiency can enhance alcohol-induced intestinal-barrier dysfunction (b). (a) Effect of zinc deprivation on the epithelial barrier of Caco-2 cells. Caco-2 cells were cultured on inserts and treated with N,N,N′,N′-tetrakis (2-pyridylmethyl) ethylenediamine (TPEN) at 2, 3, and 4 µM or 4 µM TPEN plus 100 µM zinc for 24 hours. The epithelial barrier function was assessed by measuring transepithelial electrical resistance (TEER) and FD-4 permeability. Results are means ± SD (n = 8). Significant differences (P < .05, analysis of variance [ANOVA]) are identified by different letters, a–e. T, TPEN. (b) Sensitizing effect of zinc deprivation on alcohol-induced epithelial barrier dysfunction. Caco-2 cells were cultured on inserts and treated with TPEN at 2 µM for 24 hours, followed by treatment with 5% (vol/vol) ethanol for 5 hours. The epithelial barrier function assessed by measuring TEER and FD-4 permeability. Results are means ± SD (n = 8). Significant differences (P < .05, ANOVA) are identified by different letters, a–c. From Zhong et al.100
Although the beneficial effects of zinc as an adjunct antiviral therapy for hepatitis C appear to be limited, there is promising evidence that zinc may decrease liver injury and provide antifibrotic effects in patients with chronic HCV. Himoto and coworkers107 used polaprezinc as an antifibrotic therapy in patients with chronic hepatitis C and showed a decrease in noninvasive fibrosis markers. Subsequently, Matsuoka and coworkers116 treated chronic HCV patients for 3 years with polaprezinc 150 mg bid. Zinc therapy was associated with improvement of aspartate aminotransferase (AST) and alanine aminotransferase (ALT). Interestingly, patients with lower zinc concentrations showed later reduction in liver enzymes following zinc supplementation. There was also a suggestion that the risk for hepatocellular carcinoma (HCC) may also be lower in zinc-supplemented patients.
Results from these early human studies have been supported by a variety of in vitro and animal research documenting a critical role for zinc in multiple aspects of innate and adaptive immunity. Well-established effects of zinc deficiency include thymic atrophy, alterations in thymic hormones, lymphopenia, and compromised cellular and antibody-mediated responses, which can result in increased rates and duration of infection.72–74
Classic skin lesions around the eyes, nose, and mouth in 2 alcoholics with extremely low serum zinc levels (a, b). Skin lesions rapidly resolved in both patients with zinc supplementation. Patient 1b had encephalopathy that was initially believed to be hepatic encephalopathy. However, this resolved with zinc supplementation, documenting how zinc deficiency can cause mental disturbances. From McClain et al20 and McClain.21
Zinc deficiency occurs in many types of liver disease, especially more advanced/decompensated disease. Zinc supplementation has been best studied in experimental models of ALD where it blocks most mechanisms of liver injury, including increased gut permeability, endotoxemia, oxidative stress, excess TNF production, and hepatocyte apoptosis. Zinc may have some limited antiviral effect in HCV therapy. Importantly, zinc therapy has shown some promising antifibrotic effects in chronic HCV. The dose of zinc we currently administer is 50 mg of elemental zinc (220 mg zinc sulfate) per day orally with a meal. Because of its effects on multiple targets and its relative lack of toxicity, we tend to give zinc long-term (months to years) or at least until the serum zinc level has normalized. Multiple forms of zinc are available, with some of the most widely used including zinc sulfate, zinc gluconate, zinc acetate, zinc picolinate, and others. To our knowledge, zinc acetate is the only zinc supplement requiring a prescription, and extensive information on these supplements, including tablet dosing, is available on the Internet.
Enhance your photography with the LGT075T Diffusion Film, a customizable light guide acrylic sheet designed for uniform LED light diffusion on flat panel ...
It is unclear if these changes in serum and tissue zinc concentrations contribute to the initiation or promotion of HCC or whether they are the effects of malignant transformation. Studies are under way to try to elucidate the mechanisms underlying these phenomena. Somewhat conflicting data have emerged. Most recently, Franklin et al143 have reported a downregulation of ZIP14 gene expression and the near absence of the protein within hepatoma cells in core biopsy samples, which could explain the decrease in intracellular zinc levels in HCC. ZIP14 localizes to the cell membrane of normal hepatocytes and is a functional transmembrane transporter involved in the uptake of zinc into the cell.144,145 Thus, its downregulation may explain the decreased zinc levels in hepatoma cells. Because Zn has been proposed to have anticancer properties in multiple systems, the authors suggest that intracellular levels of zinc are downregulated early in HCC to suppress its antitumor effect. The human hepatoma cell line HepG2 does not lose the ZIP14 transporter. Interestingly, exposure of HepG2 cells to even physiologic concentrations of Zn (5 µM) inhibits their growth by about 80%.143 On the other hand, Weaver et al146 observed an upregulation of the zinc transporter ZIP4 gene expression in human and mouse HCC tissue compared with surrounding noncancerous tissue. In fact, ZIP4 protein was rarely found in noncancerous tissue, but it was abundant in the cancerous tissue. They then inhibited ZIP4 in Hepa cells (mouse hepatoma cell line) using a RNAi-expressing lentivirus vector, and this increased apoptosis and modestly slowed progression from G0/G1 to S phase when these cells were released from the hydroxyurea block into the zinc-deficient medium but not in the zinc-adequate medium. Furthermore, migration of these cells through a fibronectin-coated membrane was inhibited.146 Unfortunately, they did not measure zinc levels in these samples, so it is not known how the aberrant expression of ZIP4 in HCC tissue noted in this study affected tumor zinc levels.
by Q Liu · 2024 · Cited by 1 — Title:A Parallel Beam Splitting Based on Gradient Metasurface: Preparation and Fusion of Quantum Entanglement ... Abstract:Gradient metasurface, ...
STPcablemeaning
They are designed for clean air in the temperature range -25°C / +60°C. The optimized inlet cone along with the bionic profile of the blades reduce noise level ...
Recent studies in experimental animals and humans support the concepts of dysregulated zinc metabolism during infections and zinc deficiency increasing morbidity and mortality following infection. Work from Knoell’s laboratory showed that zinc deficiency increases systemic inflammation, organ damage, and mortality in a small animal model of sepsis.75 Using a cecal ligation and puncture model, they showed that zinc-deficient animals had increased bacterial burden, enhanced nuclear factor–κB (NF-κB)–binding activity, increased expression of NF-κB-targeted genes such as tumor necrosis factor (TNF)-α and ICAM-1, and increased acute-phase proteins. Similarly, genome-level expression profiling in patients with pediatric septic shock demonstrated that altered zinc homeostasis predicted poor outcome.76 Of the genes most prominently up- or downregulated, many play important roles in zinc homeostasis. We postulate that patients with liver disease who have underlying dysregulated zinc homeostasis will have this altered zinc metabolism exacerbated by infection or inflammation, potentially leading to poor outcome.
Metallothionein is mainly a cytosolic peptide with a high cysteine content that binds metals such as zinc and copper quite avidly (copper having a higher affinity). In the cytosol of enterocytes, metallothionein binds newly absorbed copper and prevents it from passing from the intestine into the circulation. Shed enterocytes with copper still bound to metallothionein then result in a high fecal copper content and loss of copper from the body.121–123 The dose that is frequently used for adults with Wilson disease is 50 mg elemental zinc 3 times a day. The multiple dosing regimen is critical to impair copper absorption. Many investigators have also used zinc therapy for primary treatment of Wilson disease. However, recent communications have suggested that some patients are resistant to zinc therapy.124–126 Moreover, compliance is often an issue, especially in asymptomatic patients on long-term therapy.124–126 Thus, if zinc is to be used for Wilson disease therapy (especially primary therapy), careful patient monitoring and documentation of compliance are critical. Zinc therapy is an attractive therapeutic agent because it is inexpensive and relatively nontoxic compared to chelation therapy.
Wilson disease is an autosomal recessive disorder of copper metabolism. Zinc was first used to treat Wilson disease in the Netherlands as early as the 1960s. Zinc acetate was approved for maintenance therapy by the FDA in 1997, based on research that showed that zinc caused a negative copper balance, controlled urine and plasma copper levels, removed stored copper, and protected the liver, at least in part, by inducing the expression of intestinal and hepatic metallothionein.121–123
Although we are beginning to learn about the role of zinc transporters in experimental inflammation and in human infections, no studies to date in human cirrhosis have evaluated this important topic. Expanded knowledge of intracellular zinc metabolism and the role of zinc transporters in liver disease will enhance our understanding concerning altered zinc metabolism and zinc therapeutic effects in liver disease.




 Ms.Cici
Ms.Cici 
 8618319014500
8618319014500