2.8: The Simple Magnifier - magnification lens
Case E. Middle aged man developed chronic headaches, photophobia, blurred vision, and nighttime vision difficulties 5 years after photographing a ship. He surmised that a laser caused the injury. Not due to laser injury.
As light energy reaches the retina, its deposition, penetration and/ or absorption depends on wavelength, duration of exposure, and composition of retinal tissues. When energy deposition is too low or dispersion is too high, oxidative photochemical damage occurs via absorption of photons. If deposition is greater than thermal dispersion, and resulting tissue temperature increase is greater or equal to 10°C, photothermal damage occurs. Nonlinear damage can occur via sheer stress and cavitation if energy deposition is faster than tissue relaxation. Ultra-short high energy lasers can create very precise locally extreme heat to 10,000°C, causing photodisruptive damage[34]. Tissue response to absorbed energy can include photocoagulative, photothermal, and photodynamic injury[35]. Injury types are dependent upon power density, total exposure duration, and wavelength of irradiating energy, which are effected by wavelength-dependent properties of the anterior segment and vitreous[36].
Made from high quality Schott glass and manufactured precision bonding and polishing techniques. Circular Polarizers have little noticeable optical downside ...
Compound parabolic concentratorwikipedia
A general summary of non-therapeutic laser retina injuries is presented, including information about growth of the industry, increasingly accessible online markets, inconsistent international regulation, laser classifications, laser wavelengths, and laser power, mechanisms of tissue injury, and a demonstration of the variety of settings in which injury may occur. Finally, 68 cases found in the literature are summarized to illustrate the presentations and outcomes of these patients.
Federal Aviation Administration (FAA) reports of pilot-related laser incidents rose from 2,836 in 2010 to 7,442 in 2016[115]. A 2015 Canadian article analyzed 58 male and 3 female airline pilots who reported to their clinic due to laser strike while flying between April 2012 and November 2014. All pilots reported immediate ocular irritation or light sensitivity, but there were no signs of damage documented on ophthalmic exam that included visual acuity, color vision, visual fields, intraocular pressure (IOP), slit lamp examination, dilated fundus examination, color fundus photos, and OCT[116]. Only 1 confirmed case has been published of permanent retinal injury to a pilot. It occurred from blue laser light while the plane was at an elevation of approximately 396 m. Examination revealed localized photoreceptor disruption on OCT, well-demarcated hypofluorescence on AF, and an identifiable lesion on dilated fundus examination[117]. Despite the lack of lasting ocular damage, these incidents can cause glare, flash blindness and irritation that can jeopardize the safety of the flight.
Case B. Middle-age woman momentarily exposed to ordinary laser pointer. 4 years later developed headaches, photophobia, and pains. No pathology on FA or slit lamp other than dry eye. 20/20 OU. Not likely due to laser injury.
The International Commission on Non-Ionizing Radiation Protection (ICNIRP) has guidelines for human exposure. Laser Maximum Permissible Exposure (MPE) limits are used in international safety standards. They are based on ICNIRP guidelines, and revised periodically to reflect new technology[94]. Several case reports since 1998 that describe industrial laser injuries including those involving Nd:YAG and Titanium-sapphire lasers and are summarized in Table 2[95,96,97,98,99,100,101,102,103,104,105].
2023217 — Think of it as a two-stage magnifying glass. The objective first produces an enlarged image of the object. This is very similar to taking macro shots with a ...
The United Nations 1980 Convention on Certain Conventional Weapons (CCW) Protocol IV, “Protocol on Blinding Laser Weapons,” came into force on October 13, 1995, and is the first international agreement regulating the use of lasers as weapons during combat[161]. It specifically prohibits the use of blinding laser weapons in warfare that are designed to cause permanent blindness and requires precaution to prevent blindness when non-combat laser systems are employed in combat. The agreement was the first time since the banning of explosive bullets in 1868 that the international community as pre-emptively banned a destructive technology from warfare prior to its widespread implementation on the battlefield[162]. Prior to the ban, however, laser weapons had already been developed that specifically target the eye. For instance, the U.S. developed a shoulder-mounted laser rifle with a beam diameter of 1 m and blinding range of 1 km. China had a similar, tripod-based weapon with a purported blinding range of 2 km to 3 km and the capability to sustain two simultaneous wavelengths at 15 mW for 5 minutes[159]. As of January 28, 2018, 108 nations have agreed to the treaty[160].
Children are vulnerable particularly to lasers purchased from unregulated marketplaces[121], for instance online, where they can subsequently be used for entertainment[122]. These lasers may be unsafe, over the 5mW FDA safety limit, and indistinguishable in appearance from low-powered lasers. They can produce retinal injury with momentary exposure[123]. Online marketing of these lasers seem particularly attractive to teenagers as fun gadgets, laser swords, and pranks[124].
In 1997, the United States Food and Drug Administration (FDA) warned that lasers could be “more damaging than staring directly into the sun,” and imposed regulations on laser sales[3]. That same year, the British government banned Class III lasers due to retinal damage from direct exposure[4]. In 1998, the World Health Organization (WHO) warned of handheld laser pointers that are “too powerful for general use” that pose “an unacceptable risk in the hands of consumers.”[5]. In 1999, the British Journal of Ophthalmology (BJO) published a review of laser pointers and concluded that “laser pointers, pens or key rings if used appropriately are not an eye hazard, and even if used inappropriately will not cause permanent eye damage.” Up to that point, commercially-available laser pointers had caused only temporary or reversible injury unless used deliberately for harm or stared at for long durations of time[6]. In 2001, there was debate about whether U.S. domestic lasers were compliant with federal standards[7].
Blue and UV light are more onerous at lower powers because their short wavelength induces greater action spectrum within photoreceptors[79]. Michael and Wegener estimated safe exposure times to avoid photochemical injury for different light sources based on American Conference for Governmental and Industrial Hygienists data on the Zeiss operation microscope OPMI VISU 200[80].
Are there ocular abnormalities that could have been caused by a known laser-tissue interaction at the time of the reported incident?
On the other hand, the well-controlled use of therapeutic lasers has contributed significantly to the field of ophthalmology. For example, femtosecond laser can be used to assist cataract surgery. The Diabetic Retinopathy Study (DRS) and the Early Treatment Diabetic Retinopathy Studies (ETDRS) demonstrated the benefit of panretinal and focal photocoagulation retinal laser photocoagulation in diabetic retinopathy. Laser has been the standard of care for diabetic retinopathy for decades[13,14,15]. Neodymium-doped yttrium aluminum garnet (Nd:YAG) laser hyaloidotomy can be used for rapid resolution of premacular subhyaloid hemorrhage[16]. Photodynamic therapy (PDT) utilizes injection of tissues with a contrast agent that is absorptive at specific frequencies, which when targeted initiates ablation of tissue[17]. Photocoagulation can also be used in numerous other conditions, including: retinal vein obstruction, proliferative diabetic retinopathy, retinal tears, and age-related macular degeneration, but can cause reduced night vision, scotoma, macular edema, thinning, and scarring[18].
Parabolicdish collector
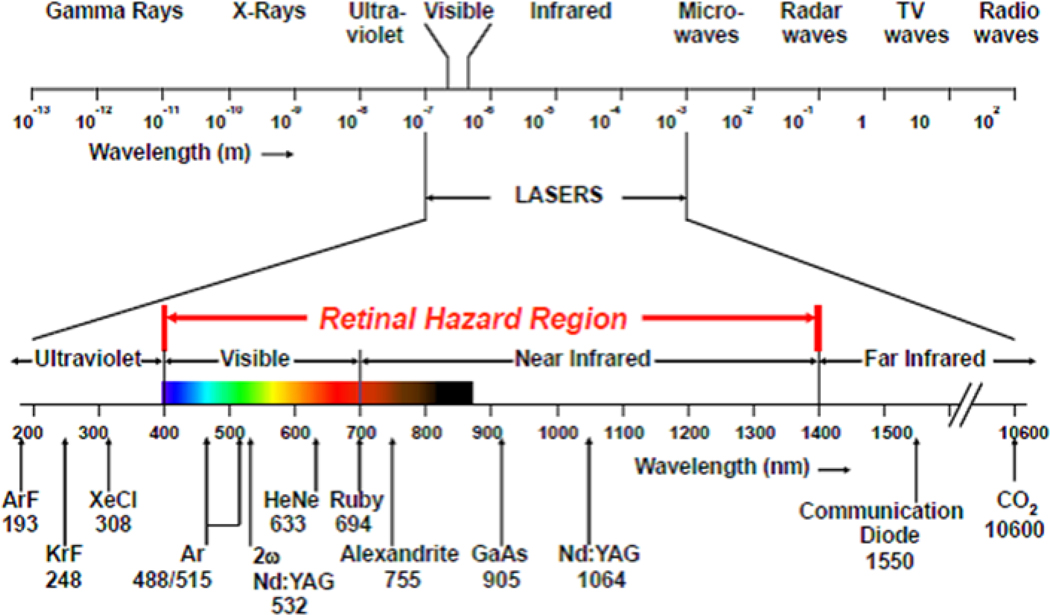
Representation of a variety of handheld, commercial, and medical laser wavelengths i. i Paulausky, C. Laser Safety: The Eyes Have It! Occupational Health & Safety. August 2, 2014. https://ohsonline.com/Articles/2014/08/01/Laser-Safety_0.aspx.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
A comprehensive literature review on the PubMed database was conducted to present case reports and case series representative of the variety of laser eye injuries in different injury circumstances, tissue types, and biological damage mechanisms.
Lasers are increasingly used for medical, industrial, commercial, military, research, and entertainment purposes, spurred by rapid technological development, decreasing size, and decreasing costs. The continued proliferation of laser use[1] and their relative ease of unregulated purchase have resulted in concern over the consequences of unintended or malicious laser eye injuries. As they have increased in popularity, so have the incidents of accidental laser use injuries[2]. Figure 1 demonstrates a handheld laser pointer that is commercially available online.
Accidental exposure to a hand-held Nd:YAG range finder laser in 2004 resulted in a full thickness foveal hole in a 20-year-old man[91]. In Oman, three soldiers celebrating a football game developed vision loss after competing in a staring contest with blue-green laser pointers lasting 5–10 seconds[92]. A 2015 Military Medicine case study presented case of “visually significant damage to the retina” from brief handheld laser exposure, and warns of dangers from increasing number of military target designating, range finding and radar warning system lasers with high powers[93]. These and other military related laser exposure cases are summarized in (Table 1).
The growing use of lasers and increasing cases of non-therapeutic laser injury underscores the importance of understanding the scope and types of non-therapeutic laser eye injuries. This review will evaluate the means and mechanisms of injury in terms of the wavelengths at risk, current policies governing laser regulations, laser principles and specific tissue injuries, imaging modalities for identifying real from imagined laser eye injuries, and cases and types of injuries reported in the literature.
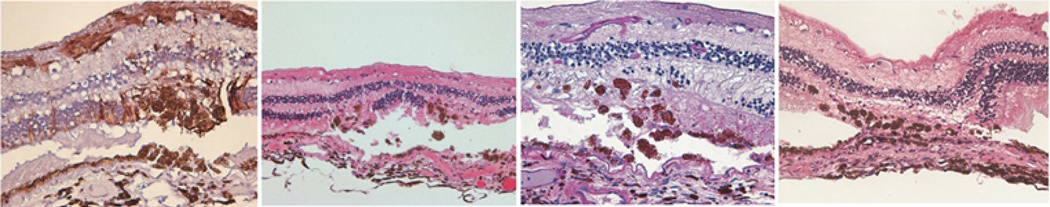
Histology of photocoagulation from semi-automated pattern scanning retinal photocoagulation (PASCAL) i. i Paulus YM, Kaur K, Egbert PR, Blumenkranz MS, Moshfeghi DM. Human histopathology of PASCAL laser burns. Eye. 2013 Aug 31;27(8):995–6.
Injury may occur at different retinal layers based upon duration, wavelength, and power of laser. For instance, green light undergoes less angular spreading than red light, making it more harmful. Green laser light (532 nm) may be additionally harmful due to its wavelength near the peak-sensitivity of dark-adapted eyes[39]. Utilizing blue light for macular photocoagulation can result in damage to the inner neurosensory retina.
If so, and substantial visual or somatic complaints are present, is there any scientific evidence that the objective ocular findings could cause the reported subjective complaints?
United States laser sales are regulated by the Food and Drug Administration Code of Federal Regulations, which requires compliance for Class I, II, IIA and IIIA devices. Many countries and international Internet sales are unregulated or unenforced[33]. For instance, a quick Internet search yields a 6 W laser available for purchase that exceeds the ANSI safety limits by greater than 20,000 times and requires only 10 milliseconds to cause damage, far faster than the blink reflex. In Europe, EN 60825/207/208 provides regulation for safe laser use and necessary protective equipment by limiting exposure respect to energy per unit of beam area with no allowance for diffuse viewing conditions. The American standard, ANSI, which has been adopted by many Asian countries, specifies protective eyewear requirements in terms of optical density (OD) and allows for a nominal hazard zone to be determined by a laser safety officer outside of which diffuse viewing eyewear is allowed. Whereas optical density requirements allow for a diffuse viewing condition, a code that regulates permissible energy density will more specifically protect against direct beam exposures and protects against diffuse exposure that rises above threshold energy limits.
The American National Standards Institute (ANSI)[24] establishes maximum permissible laser radiation exposure an unprotected person may receive without biological consequence as measured by tissue samples and imaging[25,26,27,28,29,30]. They classify lasers by output.
Photothermal damage occurs by transfer of photon energy from light to retinal molecules, provided that the difference between the molecule’s energy states is equal to that of the photon. Photothermal damage tends to occur at longer (red-shifted) wavelengths and shorter pulses, and tends to be irreversible when ambient temperature of the retina increases by 10°C. Cells may undergo apoptosis with varying degrees of necrosis up to 68°C, and immediate cell death above 72°C[70]. Photothermal absorption occurs especially within melanin (RPE melanosomes and choroid melanocytes), xanthophyll (Müller cells and neurosensory retina), and hemoglobin (retinal and choroidal blood vessels)[71]. Photothermal tissue injury is utilized therapeutically in transpupillary thermotherapy (TTT) procedures, which were introduced in 1995[72]. TTT has been applied for treatment of choroidal tumors[73], retinoblastoma, choroidal neovascularization[74], and age-related macular degeneration[75].
Typically, handheld laser pointer energy is insufficient to cause injury at the ocular surface. However, greater than 100-fold amplification of irradiance by the ocular media and focusing power of the eye make the retina particularly susceptible to laser eye injury. Anterior segment injuries from handheld lasers are rare, while blink response (average aversion time 0.25 seconds), pupillary constriction and aversion to laser light brightness are usually protective. With greater than 5 mW lasers, the power may be too great for our natural defenses, resulting in severe, permanent damage with vision loss. Minor foveal injury and macular sparing are good prognostic signs for visual recovery[21].
Photocoagulative therapy is typically performed with continuous 514–532 nm green, 577 nm yellow, or 647 nm red laser with 100–200 millisecond (ms) pulses, 100–500 micrometer spot size, and 100–750 milliwatt (mW) power. Panretinal photocoagulation has been proven to be effective at halting angiogenesis, but it can cause scarring and decreased peripheral, color, and night vision. Focal and grid laser photocoagulation are effective for treatment of macular edema, but can cause scotoma and scarring. Damage surrounding the treatment area can adversely affect patients. Complications include retinal atrophy, thinning, scotomas, post-laser lesion enlargement, choroidal neovascularization, subretinal fibrosis, and visual field loss[60]. Attempts to limit side-effects include adjusting pulse duration, spacing, intensity, and axial localization[61,62].
Pseudophakic retinas with polymethylmethacryl intraocular lenses (IOLs) may be at greater risk due to higher temperature increases and UV retinal irradiances[150]. Modern IOLs, however, are mostly made of acrylic and are designed to block numerous blue and harmful wavelengths. Direct sun gazing is likely harmful, and has been shown in rat models to cause neuronal apoptosis and glio-vascular response in the retina that can lead to permanent vision loss[151]. UV light is a risk factor for age-related macular degeneration (ARMD) [152]. Solar retinopathy has been reported during prayers[153], observing solar eclipse[154,155], during recreational sun gazing[156], sunbathing and mental disturbance[157,158].
Laser stands for Light Amplification by Stimulated Emission of Radiation. It was first developed in 1960[22]. Lasers are monochromatic, coherent, and non-divergent[23]. A laser is composed of three basic elements: an active medium, a resonant cavity, and an excitation or pumping mechanism. Specific laser properties depend on the stimulated element, molecule, or compound (Figure 2). Examples of commonly used lasers in ophthalmology include: (1) Visible spectrum (400–700 nm): Argon (blue-green and green), Krypton (yellow and red), tunable dye, helium-neon, frequency-doubled Nd:YAG; (2) Infrared: Nd:YAG and carbon dioxide (CO2); (3) Ultraviolet (UV): Excimer.
The U.N. agreement does not limit blinding as an incidental effect of non-intentionally blinding laser systems. The ban also does not remove potentially blinding equipment such as range finders and target illuminators from combat, despite their potential for use as intentionally blinding weapons. This issue was well-framed by British ophthalmologist John Marshall in BMJ in 1997, noting that a wide variety of not-specifically-weapon lasers were still being used as weapons on the battlefield[163]. Incidental injuries have also been a problem unaddressed by the agreement, as blinding lasers are still used for a variety of battlefield purposes that include range-finding, target designation, antisensors, and antimaterial systems designed to disable equipment but could be used on humans as well, in violation of the UN agreement[164–168]. Currently, there are also laser systems developed for the battlefield that intend to create a temporary glare effect in enemy soldiers, and it is likely that these anti-personnel weapons will continue to be developed[169].
Interestingly, complaints of accidental laser eye injuries are for more numerous than confirmed instances of retinal injury, with less severe cases more being difficult to diagnose. Symptoms of laser-induced ocular injury include decreased visual acuity, scotoma, photophobia, metamorphopsia, and chromatopsia. Chronic ocular, facial, and head pain are not attributed to laser pointer injury. Redness and irritation are similarly non-attributable. Signs include linear streaking and hypofluorescence on FA, and visible lesion on dilated fundus examination. AOSLO, fluorescein angiography (FA), fundus autofluorescence (FAF), OCT, and infrared (IR) have also been used to characterize lesions[88]. Mainster et al. present a 5-case series along with series of 6 questions to aid in evaluating real or imagined laser eye injury. The following question and case series can be used to aid in evaluation[89].
Wide range of Micro USB cable, e.g. for charging smartphones or data connection between phone and computer. USB Type A to Micro B.
Case A. 11-year-old girl >10 seconds staring at red laser pointer resulting in painless scotoma. Central foveal pigment mottling and faint hyperfluorescence on evaluation 3 weeks later. Vision returned to 20/25. Yes, likely due to laser injury.
Cheap/bargain filters never perform well, in my experience. It costs money to get optics/color working well and not degrade the image quality ...
Parabolictroughconcentrator
Advanced imaging technology now allows for recognition and study of previously-undetectable light-induced retinal injury and their relationship to wavelength, power, and duration[47]. Morgan et al. in 2008 demonstrated via adaptive optics scanning laser ophthalmoscope (AOSLO) retinal pigment epithelium (RPE) autofluorescence changes induced by 568-nm light exposure at a power level at or near current laser safety standards[48]. Since then, optical coherence tomography (OCT), fluorescein angiography (FA), adaptive optics (AO), and other technologies have emerged that are detecting previously-underappreciated or undetected damage[49,50]. This includes sub-RPE choriocapillaris damage[51] in subtle[52], early[53], and chronic solar retinopathy[54,55,56,57].
CPC lens
As lasers have become an increasingly important component of commercial, industrial, military, and medical applications, reported incidents of non-therapeutic laser eye injuries have increased. The retina is particularly vulnerable due to the focusing power and optical transparency of the eye. Continued innovations in laser technology will likely mean that lasers will play an increasingly important and ubiquitous role throughout the world. Critical evaluation should thus be paid to ensure that non-therapeutic injuries are minimized, recognized, and treated appropriately.
Correspondence to: Yannis M. Paulus, MD, FACS, University of Michigan Kellogg Eye Center, 1000 Wall Street, Ann Arbor, MI 48105, ypaulus@med.umich.edu, Telephone: +1-734-232-8105, Fax: +1-734-936-3815
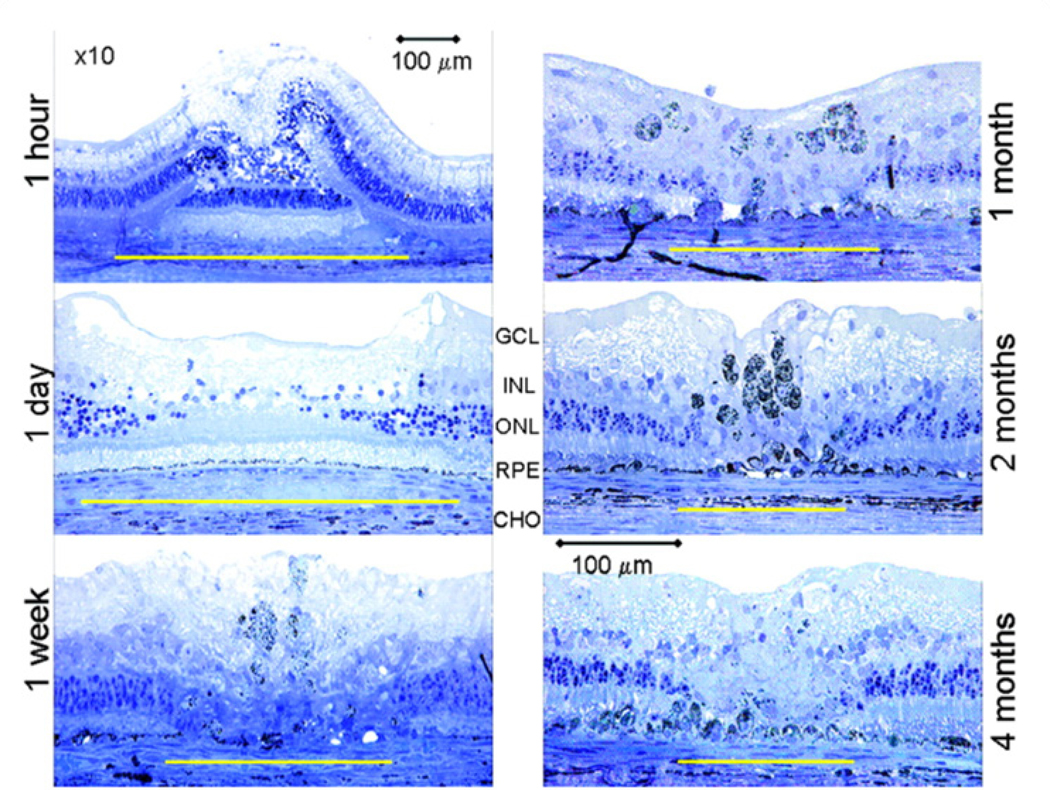
Paulus et al. illustrate rabbit histology of healing retina after 532 nm Nd:YAG photocoagulation laser injury demonstrating a permanent chorioretinal scar in moderate burns i. i Paulus YM, Jain A, Gariano RF, et al. Healing of retinal photocoagulation lesions. Invest Ophthalmol Vis Sci. 2008; 49(12):5540–5545.
Class II (< 1 mW) and Class IIIA (1–5 mW) cause retinal damage if viewed greater than 10 s at close range. These lasers rely on our natural aversion to bright lights, which is impaired for instance by altered mentation, malice, or curiosity. Class IIIA was initially thought to be innocuous unless viewed greater than 10s, but some studies in to-be-enucleated eyes have demonstrated histopathologic changes[31].
If so, have those abnormalities been documented by a reliable technique, such as fundus photography, fluorescein angiography, or optical coherence tomography?
Compound parabolic concentratorPDF
The article goes through several sample cases of applying the above 6 criteria to an evaluation of alleged laser eye injury.
Case D. 40-year-old soldier: 3 light pulses in 3 seconds by tank 3 km away. Ocular discomfort lasting 1 hour after mission, relieved by acetaminophen. Visual acuity 20/200 after incident and over next 5 years. 7 years after incident: metamorphopsia. 9 years after incident: 20/20 OD 20/50 OS. Numerous macular 50–100 μm yellow flecks OU. FA: flecks had central hypofluorescence with surrounding hyperfluorescence that faded with time. Not due to laser injury.
Photodisruption results from tissue ionization. Short bursts of high power laser pulses create acoustic shock wave and plasma, which disrupts tissue. Despite being referred to as “cold laser,” photodisruptive lasers actually create a microenvironment greater than 10,000°C. They were first used clinically in 1972 for glaucoma. They are now used in minimally invasive surgery i.e. Nd:YAG laser[86]. Near-infrared 1030–1064 nm femtosecond lasers that utilize photodisruptive tissue injury are used therapeutically in femtosecond assisted cataract surgery to add precision and reproducibility. Energy transmitted to the retina and choroid may damage these tissues due to wavelength-absorbing melanosomes in the RPE and pigmented choroid that can cause damage via microbubble formation, shock wave damage, and cumulative thermal damage[87].
The 2.5" form factor offers compatibility and ease of installation, while mSATA suits smaller devices with limited space. The M.2 form factor strikes a balance ...
Compound parabolic concentratorsolar collector
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Wavelengths between 400 nm and 760 nm are recognized as visible light, whereas wavelengths outside of this range also reach the retina. The eye is designed to focus light on the retina, primarily by the tear film, cornea, and lens. The cornea only transmits photons greater than 295 nm. The lens absorbs almost all wavelengths near 400 nm, including some blue and ultraviolet (UV) light. The lens with age absorbs more UV-A. There are lens filters that block 99% of the UV spectrum from reaching retina[19]. The retina itself has evolved to capture photons efficiently and initiate visual transduction. Overall, the focusing power and anatomical function of the eye means that retinal tissue is particularly susceptible to laser-induced injury[20].
Maximal permissible exposure times are often presented in the field of occupational health for different light sources. For instance, Okuno et al. presented a study of blue-light hazards from various light sources[113], and a systematic analysis was published specifically on light-based insect traps[114].
As non-therapeutic laser eye injuries increase in frequency, there is a greater need for public health, policy, diagnosis, and treatment of these types of injuries.
Photoswitches are photochemical pharmaceutical agents modified with an azobenzene derivative which switches between cis and trans conformations. They have been proposed as potential approaches for vision restoration in retinal degeneration[84]. Research is ongoing to develop retinal neurosensory-sparing lasers that modulate RPE transgene expression[85].
Parabolicdish collector diagram
In an Agouti rat model, blue light (405nm, 3.2mW/cm2) damage applied over 2 hours resulted in photoreceptor apoptotic death, and cellular damage in the outer retina[81]. In an early study, low power blue light (441 nm) sustained for 16.7 minutes resulted in nonthermal, photochemical damage to RPE with histological response and hypopigmentation after 48 hours[82]. RPE expresses L-type calcium channel α1D subunit, vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF) in response to blue light in vitro[83].
Photochemical injury occurs primarily in the outer layers of the central retina principally by short-wavelength exposures. It is by this mechanism that solar retinitis, iatrogenic ophthalmic instrument injury, and blue light-induced age-related macular degeneration (ARMD) are likely to occur. Cell death is via apoptosis. Injury by photochemical injury is classified as follows. Class I damage is via rhodopsin action spectrum mediated by visual pigments with primary lesions in photoreceptors. Action spectrum is heightened with higher frequency, which explains why blue lights are particularly harmful. Class II damage occurs at the RPE[78].
Argon and krypton wavelengths are primarily absorbed by hemoglobin and melanin, which then increase in temperature resulting in protein denaturation and tissue breakdown. Therapeutic applications of photocoagulative tissue injury include treatment of proliferative diabetic retinopathy, retinal vein occlusion, retinal capillary hemangioma, and choroidal tumors[59].
There is a growing research basis for understanding retinal tissue recovery following certain patterns of laser injury. Following inner retinal-neuron-sparing selective laser photocoagulation, rabbit retinal neurons exhibit plasticity by changing connectivity to restore anatomy and function[64]. The continuity of the photoreceptor layer can also be restored in rabbit and rodent models following selective photocoagulation. RPE coverage restoration takes places within days, followed by the photoreceptor layer weeks to months later[65,66]. Photoreceptors filling a lesion likely migrate from adjacent healthy areas[67,68]. c-Met facilitates RPE migratory response in response to laser-induced retinal injury[69]. (Figures 4 and 5) demonstrate histologic characteristics of semi-automated pattern scanning retinal photocoagulation and Nd:YAG photocoagulation respectively.
May 22, 2023 — The mount is the part that joins the camera's body and the lens. To shoot images, attach the lens to your camera's lens mount and let the lens ...
Compound parabolic concentratorequation
With a precision ball screw drive and intelligent stepper motor controller, you can take advantage of excellent positioning characteristics. Every system is ...
If so, do findings from ophthalmoscopy and retinal imaging evolve after the incident in a manner consistent with a laser injury?
Unlike regular glue, Bondic uses a special liquid formula that hardens when exposed to UV light. This means you don't have to wait for the glue to dry and it ...
Laser light localized to the retina is the most important determining factor for injury. Retinal injury from lasers range from subclinical to full-thickness macular holes with impaired choroidal perfusion[37]. Visual loss is greater at the fovea; peripheral injury is less symptomatic. Risk factors that increase injury include large pupil size due to increased transmission, and increased retinal and choroidal pigmentation due to the broad absorption spectrum of photon energy by melanin in the retinal pigment epithelium (RPE)[38].
If so, and substantial visual complaints are present, is the location of Amsler grid or visual field defects stable and consistent with the location of the retinal abnormalities supposedly responsible for causing them?
Industrial photoretinitis maculopathy has been described in the following settings: (1) as the result of non-ionizing radiation generated from metal arc inert gas-shielded welding and oxygen lance light[108]; (2) despite protective lenses[109,110]; (3) in the setting of fluphenazine accumulation in the RPE[111] and (4) due to light flash from short-circuited high-tension electrical circuit[112].
Modulating wavelength may also minimize certain side-effects. For example, yellow (577 nm) laser for photocoagulation may reduce the risk of Bruch’s membrane rupture as compared to 532 nm green laser[63].
Handheld laser pointers sold in the United States have generally been considered safe due to evidence-based Food and Drug Administration (FDA) regulations. However, the online marketplace is unregulated and has resulted in children using them to pop balloons and accidentally injure their eyes[119]. Pointers purchased online are not necessarily readily distinguished by the consumer, or in other cases are marketed to amateur consumers interested in high powered, unregulated lasers[120].
Certain case reports could not be included in our summary table due to lack of access, language, or formatting difficulty. They are presented here. A 2014 case series from the Netherlands describes boys aged 13, 12, and 9 who developed permanent vision loss after playing with unsafe laser pointers. One of the laser pointers was an unlabeled Class IIIB 125 mW, which was purchased while on vacation in Croatia. Another was a Class IIIA purchased during a father’s business trip in China. The other a class IIIB 5–500 mW laser was purchased in Thailand as a gift[146]. Phototoxic maculopathy has been described from staring at a quartz infrared heat lamp via photothermal and photochemical mechanisms[147]. Tomasso et al. published a 2017 paper in European Journal of Ophthalmology that first described sub-RPE (choriocapillaris) laser pointer injury via findings OCT in a 13-year-old boy who had stared into the beam of a laser pointer[148]. Laser pointers may be used by people with history of self-harm, as in a case report from France in 2016[149].
A 2014 paper from Pocock et al. in the Journal of Ophthalmology evaluated in vivo imaging of photothermal, photochemical, and photomechanical retinal laser injury in cynomolgus monkeys. They identified unique characteristics for each type of tissue injury, and noted that high resolution images are better at detecting laser eye lesions[58].
If you are unable to complete the above request please contact us using the below link, providing a screenshot of your experience.
Learn about Optical Coherence Tomography (OCT): a precise imaging tool that uses non-invasive lasers to detect eye diseases like Macular Degeneration and ...
Photochemical injury is independent of the energy transfer required for photothermal and photocoagulation. It occurs by generating free radicals from light incident on retinal tissue. It predominates at long exposures of short wavelength (i.e. blue light over time)[76]. Energy requirements for photochemical damage have also been described on a continuum with requirements for photothermal damage[77].
Military and industrial lasers injure an estimated 15 people annually. A 2003 case review series published on military laser retinal injuries included 10 cases from 1984–2000, mostly by 1064 nm q-switched Nd:YAG range finding lasers. No corneal or anterior chamber injuries were reported. No individuals were wearing eye protection. Two received medical discharges as the result of their injuries. Authors suggest that unintentional injuries may be reduced by improving operator safety training and compliance, as well as improving equipment safety design features[90].
Welders are at risk for retinal injury[106]. In fact, the most frequently reported industrial retinal injuries are from welding arcs and intense lights. However, permanent vision loss from these events are rare. The most frequent attribution for industrial accidents is lack of equipment understanding and failure to follow safety standards[107].
Case C. Young male soldier accidentally exposed to q-switched 1064 nm range finder laser pulses resulting in painless decrease in vision. At 24 hours: vitreous hemorrhage overlying 2 foveal retinal holes. At 5 days: “3 prominent chorioretinal lesions with surrounding hyperfluorescence.” Visual acuity at 18 months: 20/400. Not due to laser injury.
Tissue composition is also important in determining absorbance and resultant injury within specific layers of the retina[40]. (Figure 3) Xanthophyll pigment is concentrated in the macula and has susceptibility to blue light damage due to its peak absorbance. Xanthophyll is abundant in the retinal nerve fiber layer (RNFL), inner plexiform layer (IPL), and outer plexiform layer (OPL), leaving these tissues and the inner retina particularly susceptible[41]. Hemoglobin absorbs mostly blue, green and yellow wavelengths. Melanin absorbs broadly across the visual spectrum. Laser-induced injury pathology has been studied on eyes scheduled for enucleation[42,43], and with animal models[44,45,46].
Lasers are becoming an increasingly important component of commercial, industrial, recreational, and medical equipment. While lasers are an indispensable component in the management of diseases of the vitreous and retina and have revolutionized the treatment of many ocular conditions, lasers used for non-therapeutic purposes can cause permanent damage and blindness in the eye. With the proliferation of internet sales and cryptocurrencies which are often poorly regulated, lasers are increasingly being distributed without appropriate safety precautions taken, and people are at increasing risk for injury. The eye is particularly vulnerable to laser injury due to the focusing power of the eye and the optical transparency of the eye. Particularly since the retina is central nervous tissue that does not regenerate, this injury is of critical public health importance, especially since many of the people injured in these cases are young and thus will have to live many years with significant morbidity from these injuries. This also highlights the importance and need for further development of therapies that could treat patients who have suffered from retinal laser injury where none currently exist, particular neuroprotective, neuro-regenerative, and stem cell therapies. Continued innovations in laser technology will likely mean that lasers will play an increasingly important and ubiquitous role throughout the world, and thus critical evaluation should also be paid to ensure that non-therapeutic injuries are minimized.
Absorption spectrum of several important ocular pigments i. i Lock JH-J, Fong KCS. An update on retinal laser therapy. Clinical and Experimental Optometry. 2010;94(1):43–51.
Jul 30, 2014 — One could say the near IR pollution thing is nonsense and just get a "straight" Tiffen variable ND. Or you could go with a set of individual ND ...
If the laser source involved in the alleged injury is available or known, is it capable of producing the observed clinical findings under the reported exposure conditions?
The first commercially available lasers were red (760 nm). Soon, other wavelengths became available to allow for a greater variety of commercial applications. For instance, green lasers are visible in both day and night and good for stargazing and marking far-off targets. Blue and violet lasers reflect a spectrum of colors depending on target properties. Yellow lasers have a gold hue that is desirable for laser guide star in astronomical adaptive optics[118].
Class I (< 0.4 mW) are used in optical instruments for intrabeam viewing. They do not cause damage even with long-duration retinal exposure.
A comprehensive literature review was performed on PubMed using a variety of search terms related to laser eye injuries, handheld lasers, laser retinopathy, and laser pointer damage. What follows is a sample of cases reports found in the literature that illustrate the variety of presentations and contexts for injury.
Many of the authors made recommendations or suggestions regarding prevention and recognition of laser eye injuries. These include that the presence of outer retinal streaks suggests repeated self-harm as the cause of injury. There is an interesting assertion that although brief exposures to high-powered industrial lasers may be very painful and result in macular holes, less-powered handheld lasers can cause self-injury specifically due to lack of pain and increased duration of exposure[144]. Other authors urge for stricter rules for “uncontrolled and inappropriate use of laser instruments,” and changing the “general misperception that lasers are safe to use for entertainment purposes.”[145].
Since then, the growth of the laser industry, proliferation of online marketplace, availability of unregulated overseas lasers, and lack of awareness about laser eye injuries have placed certain patient populations at risk[8]. A 2007 Pediatric Emergency Care literature review noted that nonindustrial laser eye injuries were uncommon; that transient exposure to Class II or Class IIIA does not result in injury, whereas direct, intentional, and prolonged exposure may.”[9]. A 2013 US study found that among commercially available laser pointers labeled as 1 mW to 5 mW, 90% of green pointers and 44% of red pointers had powers greater than 5 mW, and that harmful levels of additional infrared light were reported to emanate from green handheld lasers[10]. A 2016 review article in Retina concluded that “laser eye injury caused by laser pointers/handheld laser devices is possible; however, it can be avoided by proper training and teaching. It may be necessary to restrict sale of laser pointers by imposing a minimum age and educate parents about the inherent danger of laser pointers.” Its authors noted that even at Shiley Eye Institute at the University of California, San Diego (UCSD), 3 of 4 surveyed laser pointers used in lectures had power outputs greater than the standard “safe” level of 5 mW (range from 20 to 160 mW)[11]. A 2016 Spanish Society of Ophthalmology paper concluded that “a laser pointer is never a toy and therefore cannot be left within the reach of children.”[12]. There is now general consensus in the ophthalmologic community that unregulated handheld laser pointers carry the potential to cause serious eye injury.
Conflict-of-interest statement: The author(s) declare(s) that there is no conflict of interest regarding the publication of this paper.
Official websites use .gov A .gov website belongs to an official government organization in the United States.
A variety of retina-involving cases involving commercially available handheld lasers are summarized in tables 3 and 4. These include lasers purchased overseas and online, cases from Saudi Arabia, China, Japan, Germany, Saudi Arabia, and USA, and incidents involving children shining lasers in a rear-view mirror, creating their own “laser light shows,” an individual passing out at a bar looking at an LED light, ill-advised dares, and accidents[125–143].




 Ms.Cici
Ms.Cici 
 8618319014500
8618319014500