LED Dome Lights - Model 411 - dome lights
A 2014 Canadian Agency for Drugs and Technologies in Health (CADTH) rapid response50 identified no high-quality systematic reviews or RCTs that evaluated the clinical effectiveness and safety of UV light decontamination in health care. Similarly, the Agency for Healthcare Research and Quality (AHRQ) developed a technical brief on environmental cleaning for prevention of health care–associated infections in 2015.22 While the authors made no direct conclusions on UV-disinfecting devices, they noted that comparative-effectiveness studies directly comparing modalities were limited.
One study evaluated the effect of pulsed xenon UV disinfection in the operating room on surgical site infections.38 This study found a relative rate reduction in Class I surgical site infections (RR 0.55, 95% CI 0.33–0.92), but the evaluation on Class II surgical site infections was unreliable owing to imprecise point estimates. The quality of evidence was rated as very low.
We conducted a budget impact analysis from the perspective of an Ontario hospital to estimate the cost of using portable ultraviolet (UV) disinfecting devices as an adjunct to standard environmental cleaning (i.e., manual cleaning). All costs were reported in 2017 Canadian dollars (CAD).
Largest two studies reported large reductions in HAIs, with confidence intervals excluding no effect. Smallest study found nonsignificant results and included both clinically meaningful benefits and harms. We judged evidence to have borderline imprecision.
Two before-after studies reported a reduction in hospital-acquired C. difficile infection rates when compared with manual cleaning and disinfection alone (Table 3), although one of the studies was statistically underpowered (Table 4). We assessed the quality of this evidence as very low (Table 4).
According to the manufacturer, the Tru-D disinfecting device is currently being used by three hospitals in Ontario (personal communication, Tru-D, March 29).
(((multidrug or multi-drug or antibiotic* or antimicrobial) adj (resistance or resistant)) or MDRO or MDROs or ARO or AROs).tw,kw. (192960)
Abbreviations: GRADE, Grading of Recommendations Assessment, Development, and Evaluation; RCT, randomized controlled trial; UV, ultraviolet; VRE, vancomycin-resistant Enterococcus.
Cleaning patient rooms after discharge or transfer, particularly those occupied by patients who were on contact precaution (isolation units), and patients in ICUs or surgical wards where HAIs are more likely to occur
Public and patient engagement explores the lived experience of a person with a health condition, including how the condition and its treatment affects the patient, the patient's family or other caregivers, and the patient's personal environment. Public and patient engagement is intended to increase awareness and build appreciation for the needs, priorities, and preferences of the person at the centre of a treatment program. Insights gained through public and patient engagement provide an in-depth picture of lived experience, through an intimate look at the values that underpin the experience.
The methods used within our review and the availability of evidence have several limitations. In addition to the limitations noted above for individual studies, we were unable to combine data from the various studies given the substantial clinical and methodologic heterogeneity between studies. The studies varied largely in the settings evaluated, including the type of hospital (e.g., tertiary care, community hospitals, long-term acute care), the types of hospital units (e.g., ICU, burn centre, units of leukemia and lymphoma patients), and the types of rooms that were targeted (all rooms, operating rooms, rooms of patients with contact precautions). Additionally, the type of manufacturer, the timing of disinfection, and the protocols used for both UV and manual disinfection varied between studies.
Health Quality Ontario is the provincial advisor on the quality of health care. We are motivated by a single-minded purpose: Better health for all Ontarians.
Overall baseline rates of hospital-acquired C. difficile ranged from 0.79 per 1,000 patient days to 3.16 per 1,000 patient days.
The RCT examined the effect of UV disinfection on incidence rates only among patients in “seed” rooms (rooms previously occupied by patients with colonization or infection) and reported the findings as cases per 10,000 exposure days. The data available in Ontario are limited to cases per patient days or number of admissions, but not per exposure day; thus, using these findings for an economic model proved to be impossible.
Determine if developing a lived-experience evidence stream would be of value in the evidence-based analysis phase of the health technology assessment
Last, it is unclear from this review how many devices would be needed per hospital to achieve the expected reductions in HAIs, and how adding UV disinfection would affect overall room cleaning and turnover times.
Largest study found significant reduction in MRSA rates while the other two studies found no significant difference in rates of MRSA between group: confidence intervals included both a large benefit and harm with the intervention.
Overall, all point estimates showed a reduction in hospital-acquired C. difficile rates with the addition of pulsed xenon UV disinfection, although two studies were statistically underpowered. The quality of this body of evidence was assessed as very low (Table 4).
As reported in article, otherwise rate ratio, confidence intervals, and P values were calculated from number of cases and patient days reported in study.
Circular polarization
Given the literature, clinical expert opinion, and manufacturer input, UV disinfecting devices are primarily used for the following applications:
Beyond the generalizability of results related to variations in hospital infection rates and manual cleaning and disinfection methods, several implementation considerations will affect the effectiveness of UV surface-disinfecting devices within Ontario hospitals.
Sensitivity analysis (both daytime and nighttime): 1,703 h/device yearly = (8 + 6) rooms/device daily x 365 d/y x 20 min/room = 0.82 full-time employee (assuming 52 wk/y and 40 h/wk)
Study was powered for combination of outcomes and not C. difficile alone. Estimate of effect ranges from clinically meaningful reduction to clinically meaningful increase in C. difficile infection rates.
Largest study found no difference between groups. The other three large studies had long patient follow-up period; none of the studies documented no effect. Only smallest study had confidence intervals that included no effect as well as large benefits and harms. Overall, we judged evidence as having borderline imprecision and did not rate down quality of evidence.
Similarly, it is difficult to ascertain if manual cleaning and disinfection practices within the included studies reflect Ontario best practices. Beyond stating the type of disinfectant used, most studies provided limited information on the methods used for, and compliance with, environmental cleaning practices.
One included study assessed both incident colonization and infection as outcome measure, rather than infection rate alone. We judge evidence as having no serious indirectness but note variability in hospital settings and patients was evaluated as well in outcome measures.
Polarization
This report was developed by a multidisciplinary team from Health Quality Ontario. The lead clinical epidemiologist was Milica Nikitovic-Jokic and the secondary clinical epidemiologist was Conrad Kabali, the health economist was Chunmei Li, and the medical librarian was Caroline Higgins.
We recognize that, as a system, we have much to be proud of, but also that it often falls short of being the best it can be. Plus certain vulnerable segments of the population are not receiving acceptable levels of attention. Our intent at Health Quality Ontario is to continuously improve the quality of health care in this province regardless of who you are or where you live. We are driven by the desire to make the system better, and by the inarguable fact that better has no limit.
Database: EBM Reviews – Cochrane Central Register of Controlled Trials , EBM Reviews – Cochrane Database of Systematic Reviews <2005 to January 18, 2017>, EBM Reviews – Database of Abstracts of Reviews of Effects <1st Quarter 2015>, EBM Reviews – Health Technology Assessment <4th Quarter 2016>, EBM Reviews – NHS Economic Evaluation Database <1st Quarter 2015>, Embase <1980 to 2017 Week 04>, Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) <1946 to Present>
Because there is uncertainty in the clinical benefit of this technology, there is unlikely to be an equity issue concerning this technology.
We hand-searched the reference lists of the included studies, along with health technology assessment websites and other sources, to identify additional relevant studies. No citations were added.
Study was powered for combination of outcomes and not MRSA alone. Estimate of effect ranges from clinically meaningful reduction to clinically meaningful increase in MRSA infection rates.
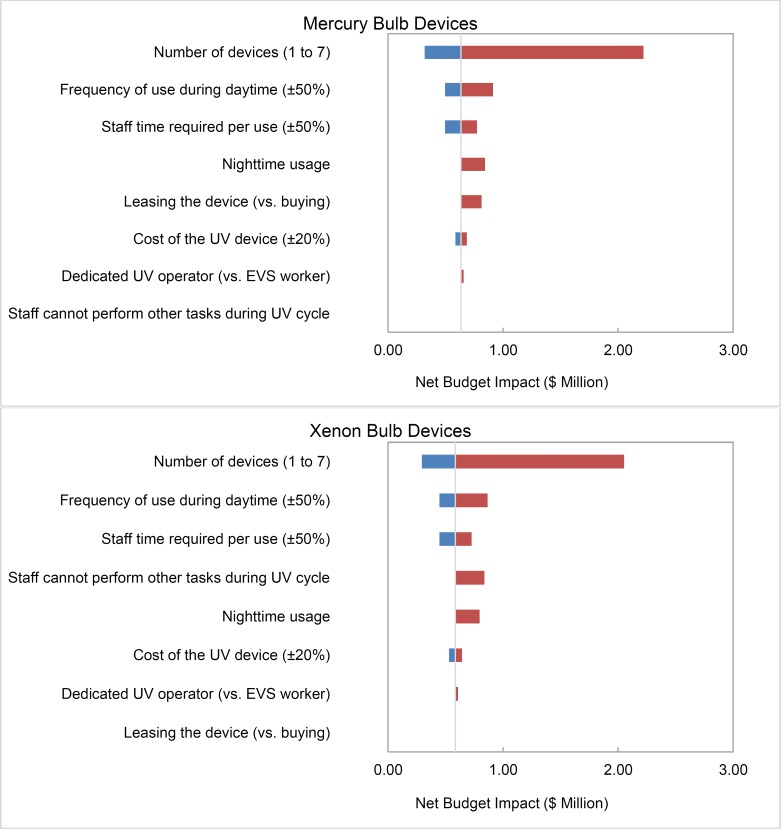
We can't be certain of the effectiveness of ultraviolet light disinfection in reducing hospital-acquired infections, given the very low to low quality of evidence. We estimated that the typical cost for a hospitals that purchases two portable devices would be $586,023 over 5 years for devices that use the pulsed xenon technology and $634,255 over 5 years for devices that use the mercury technology. Our budget impact estimates change the most if we vary our assumptions about the number of portable ultraviolet light disinfecting devices purchased per hospital, frequency of daytime use, and staff time required per use.
Nighttime usage (hospital has staff available to run the UV devices both daytime and nighttime vs. daytime only in the base case): six times/device nightly
(((Health care* or healthcare*) adj2 (acquired or associated) adj2 (infection* or disease* or pathogen*1)) or (cross adj2 (infection* or disease* or pathogen*1)) or HAI or HAIs or HCAI or HCAIs or nosocomial*).tw,kw. (91671)
(((health or healthcare or care or medical) adj2 (facility or facilities or center* or centre* or setting* or institution*1)) or hospital*1 or ((healthcare or health care) adj environment*1) or (room*1 adj2 (patient* or private or semi-private or semiprivate or recovery or isolation)) or ward or wards or ((intensive or critical) adj2 unit*) or ICU or ICUs or acute care).ti,ab,kf. (2972848)
Keywords used: ultraviolet or ultra violet or uv or uvc or uv-c or uvgi or xenon or mercury or mercure, cleaning or disinfect or disinfecting or disinfection or decontamination or terminal
With a mercury bulb device, 15 to 25 minutes is required for a vegetative cycle (e.g., for MRSA and VRE), 20 to 40 minutes for a spore cycle (e.g., for C. difficile), 60 to 75 minutes for an operating room (personal communication, March 30, 2017). We assumed that an EVS worker can clean other areas while the UV device is running, because the disinfection process requires only a single cycle/placement and the time interval is sufficiently long.
Risk of Biasa Among Randomized Controlled Trials for Comparison of UV-C Disinfection as Adjunct to Manual Cleaning and Disinfection Versus Manual Cleaning and Disinfection
We excluded studies looking at only reduced microbial contamination outcomes (i.e., reduction of surface contamination).
Abbreviations: C. difficile, Clostridium difficile; CI, confidence interval; GRADE, Grading of Recommendations Assessment, Development, and Evaluation; SD, standard deviation; OR, operating room; PXUV, pulsed xenon ultraviolet; UV, ultraviolet.
Given these limitations, substantial uncertainty about the most effective and appropriate use of these UV surface-disinfection devices remains.
The time required for UV devices to run depends on the complexity of the room (e.g., large vs. small, difficult shapes, patient room vs. operating room), type of cleaning needed (e.g., spore vs. bacteria, or C. difficile vs. MRSA/VRE) and type of UV device (mercury vs. xenon) (Table 14).
(cleaning or decontamin* or disinfect* or dis-infect* or terminal or no-touch or non-manual or germicid* or bactericid* or fungicid* or virucid* or bacteriostat*).ti,ab,kf. (1041655)
Michael W. Davidson - National High Magnetic Field Laboratory, 1800 East Paul Dirac Dr., The Florida State University, Tallahassee, Florida, 32310.
Official websites use .gov A .gov website belongs to an official government organization in the United States.
We define the meaning of quality as it pertains to health care, and provide strategic advice so all the parts of the system can improve. We also analyze virtually all aspects of Ontario's health care. This includes looking at the overall health of Ontarians, how well different areas of the system are working together, and most importantly, patient experience. We then produce comprehensive, objective reports based on data, facts and the voice of patients, caregivers and those who work each day in the health system. As well, we make recommendations on how to improve care using the best evidence. Finally, we support large scale quality improvements by working with our partners to facilitate ways for health care providers to learn from each other and share innovative approaches.
Rate ratio and confidence intervals calculated from rate data provided in article. Note that study found no statistically significant reduction between groups (P = .07) based on the Wilcoxon rank sum test.
Methods (e.g., study design, study duration and years, participant or room allocation, allocation sequence concealment, blinding, reporting of missing data, reporting of outcomes, and whether or not the study compared two or more groups)
Only Anderson et al40 summarized characteristics of patients residing within rooms that were disinfected with UV-C after manual cleaning and disinfection. The study included a total of 21,395 patients exposed to seed rooms across four study arms. Overall, patient demographics and comorbidities were similar for all cleaning strategies.
We excluded studies comparing UV with alternative devices used for no-touch room disinfection (e.g., hydrogen peroxide fogging) or where the manual cleaning and disinfection methods varied between the intervention and comparator arm of the study.
For each use, we estimated that a minimum of 20 minutes would be required to move the UV device into a room for disinfection, set up the room (e.g., staging the furniture and clinical equipment within the space to receive maximum UV exposure; placing the UV device at the optimal location; placing safety signs and a motion sensor at the entrance), and activate the machine (Table 14).
Mercury UV-C devices use low-pressure mercury gas bulbs that primarily emit a strong narrow band of the UV-C spectrum (e.g., at 254 nm). These devices use a dose targeted for the type of bacteria on surfaces (i.e., vegetative bacteria or spores). Various mercury UV-C devices exist, all of which differ on the number of lamps used and the type of output produced (e.g., standard-or maximum-output mercury lamps). As with the pulsed xenon UV devices, rooms must be vacated before disinfection, and effectiveness is limited by shadowed areas of the room. To maximize exposure to areas outside of direct line of sight, the device is typically placed in the centre of the room, with the bathroom door left open (personal communication, Tru-D, Mar 2017). Some manufacturers recommend multiple cycles from different locations, while others, such as the Tru-D Smart UVC system, disinfect rooms from a single location by using sensors to measure the amount of UV-C reflected back to the device.29 These devices stop automatically when all of the sensors meet the target dose set for the type of bacteria in the room.29 Similar to the pulsed xenon devices, mercury UV devices are generally built to stop operation if the door is opened or movement is detected in the room. Devices vary in the time to disinfect room, generally requiring upward of 45 minutes for a single cycle.
Nighttime disinfection of operating rooms, endoscopy suites, equipment supply rooms, and other high-use rooms that are typically vacant at night
Abbreviations: GRADE, Grading of Recommendations Assessment, Development, and Evaluation; MRSA, methicillin-resistant Staphylococcus aureus; RCT, randomized controlled trial; UV, ultraviolet.
economics, medical/ or economics, pharmaceutical/ or exp economics, hospital/ or economics, nursing/ or economics, dental/ (787305)
Hospital-acquired infections (HAIs) are infections that patients contract while in the hospital that were neither present nor developing at the time of admission. In Canada an estimated 10% of adults with short-term hospitalization have HAIs. According to 2003 Canadian data, between 4% and 6% of these patients die from these infections. The most common HAIs in Ontario are caused by Clostridium difficile. The standard method of reducing and preventing these infections is decontamination of patient rooms through manual cleaning and disinfection. Several portable no-touch ultraviolet (UV) light systems have been proposed to supplement current hospital cleaning and disinfecting practices.
Intervention and comparator (e.g., type of device, manufacturer, number of devices in hospital, protocol for disinfection, manual disinfection techniques and protocols used, other hospital disinfection initiatives under way)
The objective of this study was to estimate the 5-year budget impact of using portable UV disinfecting devices as an adjunct to standard environmental cleaning from an Ontario hospital perspective.
Pulsed xenon UV devices use xenon lamps to produce a flash of full germicidal light across the entire disinfecting spectrum (wavelengths of 200–320 nm; including both UV-B and UV-C spectrum), which is delivered in millisecond pulses.27
The 5-year budget impact was estimated to be $586,023 and $634,255 in Ontario hospitals (assuming two UV devices were purchased). First-year cost was the highest because of purchasing the devices ($304,708 or $340,324). Cost in subsequent years was generated by maintenance and operation of the devices (between $55,675 and $82,387 annually). Budget impact results were sensitive to the number of devices purchased by the hospital, frequency of use during daytime, and staff time required per use.
Four studies reported on hospital-acquired VRE infection rates (two evaluated mercury UV-C devices and two pulsed xenon UV devices) (Table 9). Of the two studies evaluating mercury UV-C devices, one reported the composite outcome of colonization and infection.43 Overall baseline rates of hospital-acquired VRE ranged from 0.34 per 1,000 patient days to 6.34 per 1,000 patient days.
Given this device is not applied directly to patients, a patient population of interest was not specified. We included all studies assessing the intervention in the hospital setting. All types of hospital units were included (e.g., intensive care units [ICUs], burn units, and pediatric units).
The study by Napolitano et al41 found reductions in the relative rates of hospital-acquired Acinetobacter baumanni or Klebsiella pneumoniae after the use of mercury UV disinfection versus a pre-period without UV disinfection, but the study was not adequately powered.
Risk of bias assessed using Effective Practice and Organisation of Care (EPOC) criteria for interrupted time-series studies.31
Study did not meet optimal information size, with confidence intervals that spanned both a large clinical benefit and harm.
Both included studies were reflective of the research question, although one study included both colonizations and infections contributing to increased length of stay in outcome assessment while the other study evaluated only infections. We judge evidence as having no serious indirectness but note variability in outcome definitions, use of manual disinfectants (one study did not specify disinfectant used), and hospital units evaluated (one study focused on inpatient units of leukemia and lymphoma patients, the other study on all acute care units).
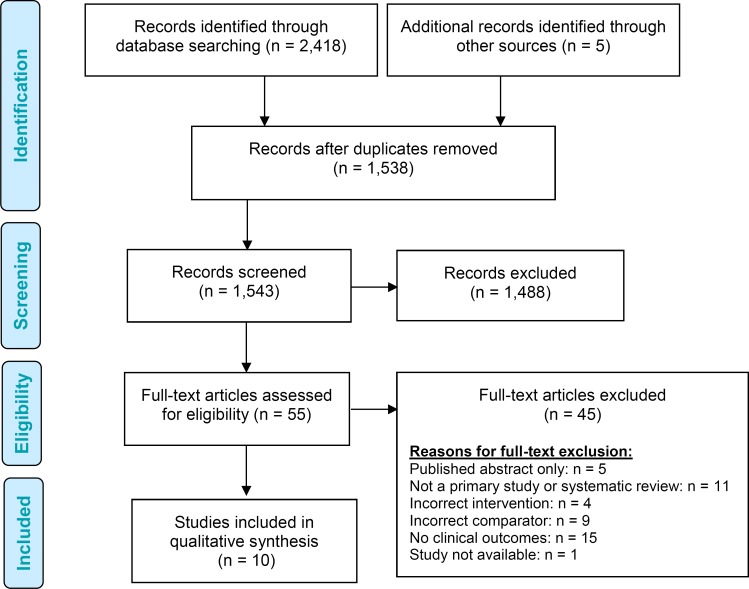
The literature search yielded 1,538 citations published between inception and January 23, 2017 after removing duplicates. We reviewed titles and abstracts to identify potentially relevant articles. We obtained the full texts of these articles for further assessment. Ten studies (one cluster RCT, one time-series analysis, and eight uncontrolled before-after studies) met the inclusion criteria.
The observational studies found in the clinical evidence review are considered very low quality evidence and therefore could not be used for an economic evaluation. Also, clinical experts suggested results of observational studies might not be generalizable to Ontario. Most of the studies were in high-incidence settings, and it is unclear whether the reduction in infection would apply in lower-incidence settings like Ontario.
(cost* adj2 (util* or efficacy* or benefit* or minimi* or analy* or saving* or estimate* or allocation or control or sharing or instrument* or technolog*)).ab. (174564)
(((multidrug or multi-drug or antibiotic* or antimicrobial) adj (resistance or resistant)) or MDRO or MDROs or ARO or AROs).ti,ab,kf. (188059)
Among studies evaluating mercury UV-C devices, the RCT by Anderson et al43 found a non– statistically significant relative reduction in hospital-acquired MRSA colonization or infection rates based on low quality of evidence (Table 8). Results from this study did find a statistically significant relative rate reduction of 33% in a separate per-protocol analysis (RR 0.67 [95% CI 0.48–0.94; P = .019]).
These technologies do not require approval by Health Canada; they are not classified as medical devices because they do not come into contact with patients during use.
Abbreviations: CI, confidence interval; ESBL, extended-spectrum β-lactamase; MDR, multidrug resistant; MRSA, methicillin-resistant Staphyloccocus aureus; VRE, vancomyocin-resistant Enterococcus, UV, ultraviolet.
Research questions are developed by Health Quality Ontario in consultation with patients, health care providers, clinical experts, and other health system stakeholders.
We performed a literature search on January 23, 2017, to retrieve studies published from inception to the search date. We used the Ovid interface to search the following databases: MEDLINE, Embase, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Health Technology Assessment, National Health Service Economic Evaluation Database (NHSEED), Database of Abstracts of Reviews of Effects (DARE); and we used the EBSCO host interface to search the Cumulative Index to Nursing & Allied Health Literature (CINAHL).
We are uncertain about the effectiveness of portable ultraviolet light disinfection devices when combined with standard hospital room cleaning because of low to very low quality of evidence. The highest quality of evidence came from the only cluster RCT evaluating the use of a mercury UV-C device for disinfection of rooms after patients with contact precautions were discharged or transferred. This study found UV disinfection to be effective at reducing the combined rate of HAI and colonization for multiple organisms (GRADE: low), but did not find a relative rate reduction on C. difficile infections and colonization (GRADE: low). While the point estimates for relative rates on VRE and MRSA favoured UV room disinfection plus manual cleaning and disinfection, we are uncertain about these estimates because they are imprecise (GRADE: low).
We performed an economic literature search on January 24, 2017, for studies published from inception to the search date. To retrieve relevant studies, the search was developed using the clinical search strategy with an economic filter applied.
All studies were conducted in hospitals within the United States. Four studies limited the use of the device and assessment of HAIs to specific units within the hospital (i.e., inpatient rooms of leukemia and lymphoma patients,44 inpatient rooms and operating rooms of a burn centre,39 operating rooms,38 or acute care units),41 while the remainder evaluated use of the device throughout all hospital units (Table 1).
(cleaning or decontamin* or disinfect* or dis-infect* or terminal or no-touch or non-manual or germicid* or bactericid* or fungicid* or virucid* or bacteriostat*).tw,kw,dv. (1046993)
polarization中文
Six of the studies reported direct conflicts of interest with, or funding received from, the manufacturer of the device38–42 or the manual cleaning agent.43 Three of the studies had coauthors who were employed by the manufacturer.38,40,42
Databases searched: EBM Reviews – Cochrane Central Register of Controlled Trials , EBM Reviews – Cochrane Database of Systematic Reviews <2005 to January 18, 2017>, EBM Reviews – Database of Abstracts of Reviews of Effects <1st Quarter 2015>, EBM Reviews – Health Technology Assessment <4th Quarter 2016>, EBM Reviews – NHS Economic Evaluation Database <1st Quarter 2015>, Embase <1980 to 2017 Week 04>, Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) <1946 to Present> Search Strategy:
We performed a qualitative synthesis of the included studies using text and tabular summaries of data. Results for studies using pulsed xenon UV disinfecting devices were summarized separately from those using mercury bulb UV-C disinfecting devices. We had planned to quantitatively synthesize studies using a priori meta-analysis; however, this analysis was not performed given substantial heterogeneity in study design, interventions, comparators, and outcome measures across the studies. Rate ratios of HAI between the manual cleaning and disinfection arms and the UV disinfection arms were taken as reported in the studies, or were otherwise calculated from data reported in the study using Review Manager Version 5.3 software.
The medical editor was Elizabeth Jean Betsch; others involved in the development and production of this report were Harrison Heft, Kellee Kaulback, Ana Laing, Claude Soulodre, Sarah McDowell, Andreé Mitchell, Vivian Ng, Anil Thota, Nancy Sikich, and Irfan Dhalla.
A single uncontrolled before-after study41 showed a 34% relative rate reduction in the combined HAIs during the follow-up period with the addition of UV disinfection. The quality of this body of evidence was assessed as very low (Table 5).
Statistically significant reduction in the combined HAI and colonization relative rate (low quality of evidence from one cluster RCT)
Ultraviolet devices are used for post-discharge or transfer cleaning rather than daily cleaning because the room must be empty of patients and staff during UV treatment. For the same reason, it is challenging to use UV devices to clean multibed rooms (vacated by one patient but still occupied by others), which are common in Canadian hospitals. Although some manufacturers provide rolling screens or blackout curtains to block the UV light and create isolation, it is very time-consuming to set them up (according to clinical experts with experience using UV devices). It is also inconvenient for patients on the other side of the room (e.g., they could need to receive care or go to the bathroom while the room is being treated with UV).
Five studies reported on HAI rates for a combined number of pathogens (Table 5). All studies included C. difficile and MRSA in their estimates, and four of the five studies included VRE. Other pathogens included in the assessment of the combined HAIs varied across studies.
Based on very low quality of evidence, one uncontrolled before-after study found a small but non–statistically significant reduction in hospital-acquired VRE rates with the use of UV-C disinfection when compared with manual cleaning and disinfection alone (Table 10).
For the base case, we assumed that two devices would be purchased by a hospital. This is consistent with most observational studies in the United States.38,45,56 According to the manufacturer, a hospital usually purchases one to two devices initially to test in some areas of the hospital (e.g., isolation ward, operating rooms), and sometimes purchases more later if staff decide to use UV disinfection for the entire hospital. Therefore, we tested a range of one to seven devices per hospital in sensitivity analysis.
The main limitation of the analysis is our inability to estimate potential cost savings from reduced HAIs, owing to uncertainty about the clinical effectiveness of UV disinfecting devices. If UV disinfecting devices do substantially reduce HAIs, they might save hospitals money. We also did not estimate costs related to increased room turnaround time or any change in patient satisfaction before and after using UV.
polarization极化
Several reviews of environmental studies have demonstrated reductions of common pathogens (e.g., MRSA, CPE, VRE, and C. difficile) on both porous and nonporous hospital surfaces with the use of both mercury UV-C and pulsed xenon UV devices.22,28 These results, however, cannot be directly extrapolated to improved patient outcomes (i.e., reduced HAI rate).
Risk of Bias Among Interrupted Time Series Studies for Comparison of UV-C Disinfection as Adjunct to Manual Cleaning and Disinfection Versus Manual Cleaning and Disinfection
We determined the usefulness of each identified study for decision-making by applying a modified applicability checklist for economic evaluations that was originally developed by the National Institute for Health and Care Excellence (NICE) in the United Kingdom. The original checklist is used to inform development of clinical guidelines by NICE.54 We retained questions from the NICE checklist related to study applicability and modified the wording of the questions to remove references to guidelines and to make questions Ontario specific. The number of studies judged to be directly applicable, partially applicable, or inapplicable to the research question are summarized.
Five studies reported on the actual use of the device, which ranged from 22% to 80% of eligible discharges (data not shown).33,38,40–42
We did not conduct a primary economic evaluation for ultraviolet (UV) disinfecting devices because the clinical evidence available did not provide precise enough estimates for the economic evaluation to be informative.
The UV room disinfection devices currently available are mobile (on casters) and can be used anywhere disinfection is desired. Given the need for the room to be empty before running the device, primary application has been targeted for cleaning rooms after patient discharge or transfer, specifically rooms of patients with contact precautions. Other proposed applications include bathrooms and shower areas, emergency departments, or operating theatres.
Other costs, such as training for cleaning personnel to use the UV devices (approximately 2 hours of staff time), are minimal and therefore were not included.
The base case results of our analysis are presented in Table 15. If a hospital decided to purchase two UV disinfecting devices, the 5-year budget impact was estimated to be $586,023 for xenon bulb devices and $634,255 for mercury bulb devices. About 53% to 56% of the total 5-year budget impact was associated with the cost of the device and warranty, and the remaining costs were associated with increased staff time for operating the devices. If a hospital decided to buy the devices, the first year's cost would be more substantial than subsequent years.
In Canada approximately 10% of adults with acute hospitalizations are estimated to have a nosocomial infection.3 Based on 2003 data, an estimated 200,000 Canadians acquire a health care–associated infection annually, with an estimated 8,000 to 12,000 persons dying as a result of their infection.3 In fiscal year 2015/16, the C. difficile infection rate for Ontario hospitals was 0.26 per 1,000 inpatient days, ranging from 0.0 to 2.94 per 1,000 inpatient days between July and August 2016.4,7 The MRSA bacteremia rate for fiscal year 2015/16 was 0.018 per 1,000 inpatient days, ranging from 0.0 to 0.235 per 1,000 days across Ontario hospitals, and the VRE bacteremia rate was 0.006 per 1,000 inpatient days, ranging from 0.0 to 0.068 per 1,000 inpatient days4 (internal data from Health System Performance at Health Quality Ontario; Data source: Health Analytics Branch, Ministry of Health and Long-Term Care, 2016). Data from the Canadian Nosocomial Infection Surveillance Program (CNISP), which are not limited to bacteremia, used 2014 national data to calculate health care–acquired MRSA infection incidence rates of 0.17 per 1,000 patient days and VRE infection incidence rates of 0.045 per 1,000 patient days.8
In subgroup analysis, Vianna et al42 found a reduction in relative rates of C. difficile in both ICU and non-ICU settings. However, the reduction was statistically significant only when limited to the non-ICU setting (RR 0.60 [95% CI 0.41–0.89]; P = .01) and not the ICU setting alone (RR 0.50 [95% CI 0.19–1.57]; P = .26). Conversely Nagaraja et al found a statistically significant reduction only when limiting analysis to the ICU setting (RR 0.30 [95% CI 0.15–0.57]; P < .001), with no significant differences observed for non-ICU, oncology, or pediatric settings.
Rate ratio, confidence intervals, and P values were otherwise calculated from number of cases and patient days reported in study.
Base case (daytime only): 973 h/device yearly = 8 rooms/device daily x 365 d/y x 20 min/room = 0.47 full-time employee (assuming 52 wk/y and 40 h/wk)
Various manual cleaning definitions were reported in each of the studies (Table 2). Only the RCT by Anderson et al43 provided detailed information regarding the standardization of room disinfection strategies after patient discharge or transfer. Four studies did not specify the cleaning agents used for standard cleaning or disinfection of rooms.38,39,41,42 Five studies specifically used bleach for cleaning of C. difficile in occupied rooms,39,40,42–44 and one used an unspecified chlorine-based product.45 Anderson et al43 used quaternary ammonium for occupied rooms in which C. difficile had not been found. Nagaraja et al33 and Haas et al32 used bleach-based solutions for all rooms except for daily cleaning of rooms with pediatric patients.35,36 Levin et al45 used a pH7Q Ultra hospital-grade disinfectant.
Rate ratio, confidence intervals, and P values were otherwise calculated from the number of cases and patient days reported in study. When no events were observed in either pre- or post-group, 0.5 was added to each cell to calculate rate ratios.
Nine studies reported on hospital-acquired C. difficile infection rates (three evaluated mercury UV-C devices and six evaluated pulsed xenon UV devices) (Table 3). Eight of the studies used a bleach product to manually disinfect rooms of patients discharged with C. difficile, and one did not specify the type of disinfectant used.
Circularlypolarized light
Based on very low quality of evidence from observational studies, pulsed xenon UV surface disinfection (when used as an adjunct to standard manual cleaning and disinfection) was associated with:
(econom* or price or prices or pricing or priced or discount* or expenditure* or budget* or pharmacoeconomic* or pharmaco-economic*).tw. (761935)
(((multidrug or multi-drug or antibiotic* or antimicrobial) adj (resistance or resistant)) or MDRO or MDROs or ARO or AROs).tw,kw. (192950)
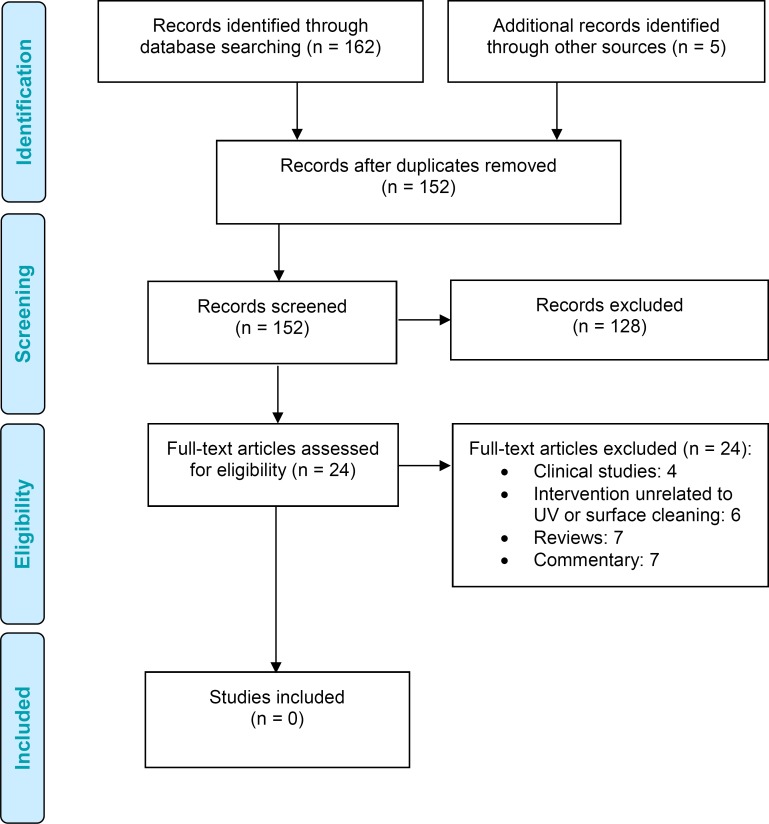
The literature search yielded 152 citations published from inception to January 24, 2017, after removing duplicates. We excluded a total of 128 articles on the basis of information in the title and abstract. We then obtained the full text of 24 potentially relevant articles for further assessment. We did not find any studies that met the inclusion criteria. Figure 2: PRISMA Flow Diagram—Economic Search Strategy presents the flow diagram for the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA).
(cost* adj2 (util* or efficacy* or benefit* or minimi* or analy* or saving* or estimate* or allocation or control or sharing or instrument* or technolog*)).ab. (174564)
Reduction in Hospital-Acquired C. Difficile Infection Rates for UV Disinfection Plus Manual Disinfection Versus Manual Disinfection Alone
Polarization of light is very useful in many aspects of optical microscopy. The microscope configuration uses crossed polarizers where the first polarizer (termed: the polarizer) is placed below the sample in the light path and the second polarizer (termed: the analyzer) is placed above the sample, between the objective and the eyepieces. With no sample on the microscope stage, the light polarized by the polarizer is blocked by the analyzer and no light is visible. When samples that are birefringent are viewed on the stage between crossed polarizers, the microscopist can visualize aspects of the samples through light rotated by the sample and then able to pass through the analyzer. The details of polarized light microscopy are thoroughly discussed in our microscopy section of this primer.
An excellent example of the basic application of liquid crystals to display devices can be found in the seven-segment LCD numerical display (Figure 3). Here, the liquid crystalline phase is sandwiched between two glass plates that have electrodes attached similar to those depicted in the illustration below. In figure 3, the glass plates are drawn with seven black electrodes that can be individually charged (these electrodes are transparent to light in real devices). Light passing through polarizer 1 is polarized in the vertical direction and, when no current is applied to the electrodes, the liquid crystalline phase induces a 90 degree "twist" of the light and it can pass through polarizer 2, which is polarized horizontally and is perpendicular to polarizer 1. This light can then form one of the seven segments on the display.
Abbreviations: GRADE, Grading of Recommendations Assessment, Development, and Evaluation; HAI, hospital-acquired infection; RCT, randomized controlled trial; UV, ultraviolet.
Risk of bias assessed using modified version of National Institutes of Health National Heart, Lung and Blood Institute's quality assessment tool for before-after (pre-post) studies with no control group.33
We judge evidence as having no serious indirectness but note variability in hospital settings and patients was evaluated as well as in outcome measures.
This type of polarized light is often termed glare and can be easily demonstrated by viewing the distant part of a highway on a sunny day. The reflection and polarization of light according to the Brewster theory can be more thoroughly examined with our Brewster Angle Java Tutorial. Light reflected by the flat surface of a highway is partially polarized with the electric field vectors vibrating in a direction that is parallel to the ground. This light can be blocked by polarizing filters oriented in a vertical direction as illustrated below in Figure 2 with a pair of polarized sunglasses.
Linear polarization
Study was powered for combination of outcomes and not VRE alone. Estimate of effect ranges from very large reduction to increase in methicillin-resistant Staphylococcus aureus infection rates.
Effect estimate had wide confidence intervals ranging from large reduction in MRSA rates to large increase in MRSA rates.
(((ultraviolet or ultra-violet or xenon or mercury or uv or uvc or uv-c) adj3 (irradia* or pulse* or emitting or lamp* or bulb* or system* or device* or robot*1)) or uvgi or px-uv or pxuv).tw,kw,dv. (67194)
Search strategies were developed by medical librarians using controlled vocabulary (i.e., Medical Subject Headings) and relevant keywords. The final search strategy was peer-reviewed using the PRESS Checklist.30 Database auto-alerts were created in MEDLINE, Embase, and CINAHL and monitored for the duration of the health technology assessment.
In comparison with standard manual cleaning and disinfection protocols alone, we found the addition of mercury UV-C room disinfection to result in:
Statistically significant reduction (one study) or a non–statistically significant increase (two studies) in MRSA infection rates
(cleaning or decontamin* or disinfect* or dis-infect* or terminal or no-touch or non-manual or germicid* or bactericid* or fungicid* or virucid* or bacteriostat*).tw,kw,dv. (1047027)
Our analysis showed that adopting UV disinfecting devices would lead to a budget impact between $586,023 (pulsed xenon) and $634,255 (mercury) over 5 years if a hospital purchases two devices. A few clinical studies reported that using UV devices could lead to cost savings from reduced HAIs. However, none of these studies have taken into account the cost of acquiring and operating UV devices. If a hospital is to adopt UV disinfecting devices, administrators must consider how many devices to acquire and whether to purchase or lease, as the up-front capital investment of purchasing UV devices can be substantial. Besides capital costs, our analysis also showed that using UV disinfecting devices as an adjunct to standard environmental cleaning would increase the workload of hospital EVS staff and could require the hospital to hire additional staff.
Most studies included in our review focused on hospitals or units with single-patient rooms. In Ontario, however, most hospital rooms are multibed rooms shared by two or more patients. The need to vacate rooms to use the device could limit use within many Ontario hospitals. The Xenex pulsed xenon UV disinfection device allows for isolation of bed spaces within multibed rooms with the use of UV black-out curtains; however, an Ontario study found that hanging the curtains was not feasible and was time-consuming.53 Clinical experts have also suggested that curtains might not be a reasonable or acceptable option because patients in the shared space must remain isolated and informed during the period of UV disinfection.
Health care–associated infections are infections that patients contract while in a health care setting (e.g., hospital, long-term care facility, emergency department, outpatient clinic, physicians' offices, community health centre) that were neither present nor developing at the time the patient was admitted. Infections that are acquired in the hospital itself are referred to as HAIs, also known as nosocomial infections. Infections are generally classified as being associated with a hospital or health care facility if they occur within 48 to 72 hours after hospitalization or visiting a health care facility, or if they appear within 10 days following discharge from hospital.1,2
The budget impact is estimated as the cost difference between two scenarios: the reference scenario (without UV disinfecting devices) and the new scenario (with UV disinfecting devices). Because UV disinfecting devices are used as an adjunct to standard cleaning, cost of standard cleaning would remain the same. Therefore, the budget impact is just the additional cost of purchasing and operating the UV devices.
The needs assessment concluded that patient engagement for this health technology assessment would be of minimal benefit and impact. A few main points were considered:
Rate ratio, confidence intervals, and P values were calculated from the number of cases and patient days reported in study. When no events were observed in either pre- or post-group, 0.5 was added to each cell to calculate rate ratios.
This health technology assessment evaluated the effectiveness and budget impact of portable ultraviolet (UV) light surface-disinfecting devices for reducing hospital-acquired infections (HAIs).
(econom* or price or prices or pricing or priced or discount* or expenditure* or budget* or pharmacoeconomic* or pharmaco-economic*).tw. (761935)
The cluster randomized trial by Anderson et al43 showed that mercury UV-C disinfection as an adjunct to manual cleaning and disinfection led to a 30% relative rate reduction in the incidence rate of infection plus colonization with one or more of the combined organisms among patients exposed to seed rooms when compared with standard cleaning and disinfection alone. The quality of the body of evidence was assessed as low (Table 6).
HTA Database Canadian Repository, Alberta Health Technologies Decision Process reviews, Canadian Agency for Drugs and Technologies in Health (CADTH), Institut national d'excellence en santé et en services sociaux (INESSS), Institute of Health Economics (IHE), McGill University Health Centre Health Technology Assessment Unit, National Institute for Health and Care Excellence (NICE), Agency for Healthcare Research and Quality (AHRQ) Evidence-based Practice Centers, Australian Government Medical Services Advisory Committee, Centers for Medicare & Medicaid Services Technology Assessments, Institute for Clinical and Economic Review, Ireland Health Information and Quality Authority Health Technology Assessments, Washington State Health Care Authority Health Technology Reviews, Tufts Cost-Effectiveness Analysis Registry, ClinicalTrials.gov
The study by Green et al39 was severely underpowered; point estimates had confidence interval that were too wide (Table 11).
Operator cannot perform other tasks while xenon UV device is running (vs. operator can perform other tasks in the base case)
The lenses of the sunglasses have polarizing filters that are oriented vertically with respect to the frames. In the Figure 2 above, the blue light waves have their electric field vectors oriented in the same direction as the polarizing lenses and, thus, are passed through. In contrast, the red light wave is perpendicular to the filters and is blocked by the lenses. Polarizing sunglasses are very useful when driving in the sun or at the beach where sunlight is reflected from the surface of the road or water leading to glare that can be almost blinding.
Natural sunlight and almost every other form of artificial illumination transmits light waves whose electric field vectors vibrate in all perpendicular planes with respect to the direction of propagation. When the electric field vectors are restricted to a single plane by filtration, then the light is said to be polarized with respect to the direction of propagation and all waves vibrate in the same plane.
We looked at randomized controlled trials (RCTs), cohort studies, and interrupted time series (also known as before-after) studies that compared UV surface disinfection.
Statistically significant reduction (three studies) or non–statistically significant reduction (two studies) in C. difficile infection rates
The Xenex Light Strike Pulsed Xenon Light Germ Zapping Robot device is currently being used in Ontario by at least two hospitals, primarily in the intensive care (ICU) and oncology units (personal communication, Xenex Disinfection Service, Feb 2017). A third hospital confirmed pilot testing the device in 2013, but discontinuing use because of problems with implementation. The pulsed xenon UV device is being tested in a trial in Saskatchewan focused on VRE.
Transmission of pathogens from environmental surfaces to patients can occur from direct infection (i.e., from an infected patient to an object and then to a subsequent patient) or indirectly (i.e., from an object to the hands of hospital staff, health care providers, or visitors to a subsequent patient). Most infections are transmitted from a prior room occupant who was infected or colonized. A prior room occupant who is infected or colonized (microorganism is present in the person, but has not invaded the tissue, or caused cellular injury, so the person shows no signs or symptoms of illness) with these pathogens has been shown to increase the risk of infection in subsequent room occupants by two times or more.17
Statistically significant reduction in the total combined HAI and colonization relative rate (very low quality of evidence from one observational study)
(((ultraviolet or ultra-violet or xenon or mercury or uv or uvc or uv-c) adj3 (irradia* or pulse* or emitting or lamp* or bulb* or system* or device* or robot*1)) or uvgi or px-uv or pxuv).ti,ab,kf. (66816)
For a health technology assessment, patient engagement can often illuminate context surrounding patient preferences for that technology and how patients make decisions surrounding its use. However, for UV disinfecting devices, the influence of patient preference on the method of choice for disinfection was negligible. Patients in acute care settings rarely are given an opportunity to express a preference for how a room is disinfected. The process is defined by the health and safety policy in the health care facility. The choice between UV disinfection and standard disinfection would most likely not be within a patient's control.
In December 2016 and January 2017, we consulted Ontario experts about UV disinfecting devices. Expert advisors included physicians and experts in the specialty areas of infectious disease prevention and control. The role of the expert advisors was to place the evidence in the context of Ontario and to provide advice on the use of UV disinfecting devices and guidelines on current standard cleaning and disinfection practices.
Specific rooms targeted for UV disinfection within hospitals varied greatly across studies. Two studies used the device for all patient rooms39,40; two studies used the device for all ICU room discharges and transfers, and for non-ICU rooms only if patients had contact precautions41,42; three studies used the device primarily for rooms of patients with contact precautions, but also used the device for other rooms and areas as appropriate or available35,36,45; two studies used the device solely for rooms of patients with contact precautions (Table 1).43,44
Similarly, several before-after studies found pulsed xenon UV disinfection devices reduced total combined HAIs, with inconsistent effects on C. difficile, MRSA, and VRE rates. The quality of the body of evidence for each outcome assessed from these studies was very low; we therefore have considerable uncertainty about these study results. One limitation is the difficulty of controlling for important confounding variables that could differ between the pre- and post-intervention periods, including the severity of illness among patients admitted, quality of medical care received, other infection control practices employed (e.g., hand-hygiene compliance), and antibiotic prescribing practices. Additionally, manual cleaning and disinfection techniques were often not described. Finally, because study investigators were not blinded to the study treatments used, we cannot know if standard cleaning and disinfection practices and protocols were enhanced when UV disinfection device protocols were implemented within the hospital.
The database search for the clinical review yielded 10 peer-reviewed publications that met eligibility criteria. Three studies focused on mercury UV-C–based technology, seven on pulsed xenon UV technology. Findings were either inconsistent or produced very low-quality evidence using the GRADE rating system. The intervention was effective in reducing the rate of the composite outcome of HAIs (combined) and colonization (but quality of evidence was low). For the review of economic studies, 152 peer-reviewed publications were identified and screened. No studies met the inclusion criteria. Under the assumption that two devices would be purchased per hospital, we estimated the 5-year budget impact of $586,023 for devices that use the pulsed xenon technology and of $634,255 for devices that use the mercury technology.
Among the mercury UV-C studies, the length of time to run the device varied with the specific device being evaluated (average time range 8–55 minutes, Table 2). For the pulsed xenon UV studies, the device was generally run three times per patient room for between 5 and 12 minutes per run. For both studies using the xenon UV device in the operating room, the device was run twice for 10 minutes each time (Table 2).
Based on very low quality of evidence, one uncontrolled before-after study found no difference in the relative rate of hospital-acquired MRSA with the use of UV-C disinfection when compared with manual cleaning and disinfection alone (Table 7).
The 10 included studies are summarized in Tables 1 and 2. Overall, substantial clinical and methodologic heterogeneity made meta-analysis inappropriate.
The studies included in this review were all performed in the United States and focused primarily on high-risk settings. Rates of baseline HAI for each of the organisms evaluated were considerably different from averages in Ontario and Canadian hospitals.4,8 It is therefore uncertain if the magnitude of effect found within the studies would be observed in Ontario.
Xenon bulb UV: for patient rooms, 18 minutes is required (three 5-minute cycles at three locations within the room; 1 minute for operator to move device); for operating rooms, 16–20 minutes is required (two 8- or 10-minute cycles).
Three studies35,39,42 found conflicting results on the effect of pulsed xenon UV disinfection on the combined HAIs (Table 6). Green et al39 evaluated both infection and incident colonizations in a burn centre with high baseline HAI rates and found no significant difference in the combined HAI rates after the device was added to manual cleaning and disinfection. This study39 had large imprecision in its estimate, likely owing to the small number of total patient exposure days. Two studies, however, found a relative rate reduction in the combined HAI rates ranging from 20% to 29% when compared with manual disinfection alone.35,42 The study by Vianna et al42 found a 61% reduction in intensive care (baseline HAI rate 6.77/1,000 patient years; rate ratio [RR] 0.39 [95% confidence interval (CI) 0.19–0.79; P = .009]), with a 22% relative rate reduction observed when limited to HAIs outside intensive care (baseline HAI rate 1.26/1,000 patient years; RR 0.78 [95% CI 0.59–1.04; P = .09]). The quality of the body of evidence for the combined HAI rates for pulsed xenon UV devices was assessed as very low (Table 6).
Our literature search did not identify any economic evaluations of UV disinfecting devices as a cleaning method in hospitals. Further research into the cost-effectiveness of UV disinfecting devices is needed.
(((health or healthcare or care or medical) adj2 (facility or facilities or center* or centre* or setting* or institution*1)) or hospital*1 or ((healthcare or health care) adj environment*1) or (room*1 adj2 (patient* or private or semi-private or semiprivate or recovery or isolation)) or ward or wards or ((intensive or critical) adj2 unit*) or ICU or ICUs or acute care).tw,kw. (2988891)
Direction and magnitude of effect was similar for two of three studies, whereas third study by Green et al39 found a non–statistically significant increase in HAI rates. Given study by Green et al was likely underpowered and had overlapping confidence intervals with the other two studies, we did not downgrade for inconsistency.
A single reviewer used DistillerSR management software to conduct an initial screening of titles and abstracts, and obtained the full text of studies that appeared eligible for the review, according to the inclusion criteria. The author then examined the full-text articles and selected studies that were eligible for inclusion.
We included studies comparing the intervention to standard hospital cleaning and disinfecting methods (i.e., manual cleaning).
Haas et al35 found a 19% relative reduction in the rate of multidrug-resistant gram-negative bacteria. Although adequately powered, this study had very serious limitations related to risk of bias (Appendix 2, Table A2).
Abbreviations: C. difficile, Clostridium difficile; GRADE, Grading of Recommendations Assessment, Development, and Evaluation; RCT, randomized controlled trial; UV, ultraviolet
(((ultraviolet or ultra-violet or xenon or mercury or uv or uvc or uv-c) adj3 (irradia* or pulse* or emitting or lamp* or bulb* or system* or device* or robot*1)) or uvgi or px-uv or pxuv).tw,kw,dv. (67193)
For this health technology assessment, the value of pursuing patient and public engagement was determined through a needs assessment by the Public, Patient, and Caregiver Engagement team at Health Quality Ontario. The purpose of this needs assessment is threefold:
Reduction in Combined Hospital-Acquired Infection Rates for UV Disinfection Plus Manual Disinfection Versus Manual Disinfection Alone
Hospital-acquired infection rates (infection only or composite outcome of infection and colonization); all HAIs were included, with a focus on but not limited to:
This concept is illustrated in Figure 1 below, and we have also constructed an interactive Java tutorial that explores the interaction of light waves with polarizers. In this example, the incident light electric field vectors are vibrating perpendicular to the direction of propagation in an equal distribution of all planes before encountering the first polarizer. The polarizers illustrated above are actually filters containing long-chain polymer molecules that are oriented in a single direction. Only the incident light that is vibrating in the same plane as the oriented polymer molecules is absorbed, while light vibrating at right angles to the plane is passed through the first polarizing filter. In Figure 1, polarizer 1 is oriented vertically to the incident beam so it will pass only the waves that are vertical in the incident beam. The wave passing through polarizer 1 is subsequently blocked by polarizer 2 because the second polarizer is oriented horizontally with respect to the electric field vector in the light wave. The concept of using two polarizers oriented at right angles with respect to each other is commonly termed crossed polarization and is fundamental to the practice of polarized light microscopy.
Non–statistically significant reduction in individual hospital-acquired MRSA or VRE infection and colonization relative rates (low quality of evidence from one cluster RCT)
Mercury bulb UV: for patient rooms, 15–25 minutes for bacteria and 20–40 minutes for spores; 60–75 minutes for operating rooms.
Risk of bias for individual studies was assessed using the Cochrane Risk of Bias tool for RCTs and the Effective Practice and Organisation of Care (EPOC) tool for non-RCTs and for interrupted time-series studies.31,32 The National Heart, Lung and Blood Institute quality assessment tool was used for before-after studies with no control group.33
Reduction in Hospital-Acquired VRE Infection Rates for UV Disinfection Plus Manual Disinfection Versus Manual Disinfection Alone
Four studies limited the assessment of HAIs to patients within the specific hospital units for which the UV device was used.38,39,41,44 The cluster RCT by Anderson et al43 evaluated outcomes only among patients who were exposed to a seed room (i.e., a room containing a patient with proven current or history of infection or colonization with one or more of the target organisms). The remainder of the studies evaluated hospital-wide HAI rates.
One of the three studies evaluated both colonization and infection with target organisms, whereas the other two specifically evaluated infection rates; we judge the evidence as having no serious indirectness but note variability in hospital settings and patients evaluated as well as outcome measures (variation in target organisms included and in definition of infection).
For these reasons, the number of rooms that can be cleaned with UV per day depends on 1) the number of isolation room discharges or transfers per day, 2) the number of private (single-bed) rooms in the hospital, and 3) the availability of staff during nights. Given staff limitations, some hospitals might be unable to use UV devices during nights. Therefore, we estimated the frequency of use on the basis of published literature,38,40–42,56 clinical expert opinion (email communication, March 18, 2017), and manufacturer input (personal communication, March 3, 2017; email communication, March 29, 2017). We estimated that, with full implementation and training, a UV device can be used for about eight patient rooms daily during the day. In sensitivity analysis, we assumed that, in addition to daytime, a device could also be used about six times nightly for operating rooms, equipment rooms, and so forth. The additional staff time needed is calculated below:
Another limitation is that all studies evaluated the effectiveness of UV disinfection devices in addition to standard cleaning, but they did not describe in detail how standard cleaning was done. For example, it would have been more informative to assess “Is doing standard cleaning twice as good as, better than, or not as good as using a UV device?”
Abbreviations: EVS, environmental services; ICU, intensive care unit; NR, not reported; OR, operating room; UV, ultraviolet.
We performed targeted grey literature searching of sites for health technology assessment agencies and clinical trial registries. See Appendix 1 for Literature Search Strategies, including all search terms.
This analysis included costs of the UV device, warranty, maintenance, and staff time required to operate the devices (Table 13). We did not include costs related to any potential reduction of HAIs, given our uncertainty about the effectiveness of UV. Cost inputs were obtained from standard Ontario sources, published literature, and the manufacturers.
Public Health Ontario and the Provincial Infectious Diseases Advisory Committee (PIDAC) have developed best practices for environmental cleaning in health care settings.1,19 Standard environmental cleaning and disinfection protocols are heterogeneous and vary according to the type of room being cleaned. Examples can include routine daily room cleaning, daily cleaning of rooms of patients with additional contact precautions (i.e., additional barrier precautions for patients with known infection or colonization, often in separate isolation units) or thorough cleaning and decontaminating of a room after patients with contact precautions were discharged or transferred.
Abbreviations: ER, emergency room; HAI, hospital-acquired infection; ICU, intensive care unit; MRSA, methicillin-resistant Staphylococcus aureus; NR, not reported; OR, operating room; PXUV, pulsed xenon ultraviolet; UV, ultraviolet; VRE, vancomycin-resistant Enterococcus.
The RCT by Anderson et al43 that used mercury UV-C devices found no difference in hospital-acquired C. difficile infection rates among patients exposed to seed rooms. The study compared disinfection with bleach plus UV-C versus disinfection with bleach alone (Table 3). We assessed the quality of this evidence as low (Table 4).
Database auto-alerts were created in MEDLINE, Embase, and the Cumulative Index to Nursing & Allied Health Literature (CINAHL) and were monitored for the duration of the health technology assessment. We performed targeted grey literature searching of sites for health technology assessment agencies, clinical trial registries, and Tufts Cost-Effectiveness Analysis Registry. See Clinical Evidence, Literature Search, above for further details on methods used, and Appendix 1 for literature search strategies, including all search terms.
Abbreviations: CI, confidence interval; OR, operating room; MRSA, methicillin-resistant Staphylococcus aureus; UV, ultraviolet.
We are a scientifically rigorous group with diverse areas of expertise. We strive for complete objectivity, and look at things from a vantage point that allows us to see the forest and the trees. We work in partnership with health care providers and organizations across the system, and engage with patients themselves, to help initiate substantial and sustainable change to the province's complex health system.
One of the most common uses of polarization today is the liquid crystal display (LCD) used in numerous applications including wrist watches, computer screens, timers, clocks, and many others. These devices are based upon the interaction of rod-like liquid crystalline molecules with an electric field and polarized light waves. The liquid crystalline phase exists in a ground state that is termed cholesteric where the molecules are oriented in layers where each successive layer is slightly twisted to form a spiral pattern. When polarized light waves interact with the liquid crystalline phase the wave is "twisted" by an angle of approximately 90 degrees with respect to the incident wave. This angle is a function of the helical pitch of the cholesteric liquid crystalline phase, which is dependent upon the chemical composition of the molecules (it can be fine-tuned by small changes to the molecules).
(((ultraviolet or ultra-violet or xenon or mercury or uv or uvc or uv-c) adj3 (irradia* or pulse* or emitting or lamp* or bulb* or system* or device* or robot*1)) or uvgi or px-uv or pxuv).ti,ab,kf. (66817)
Inconsistent results were observed among the three studies evaluating the use of pulsed xenon UV devices for prevention of MRSA infection. The point estimates for the two studies were in favour of standard manual cleaning over the addition of pulsed xenon UV disinfection, but the studies were statistically underpowered. In contrast, one study found a statistically significant relative rate reduction of 27% for pulsed xenon UV disinfection when compared with standard disinfection alone. The quality of evidence for this body of evidence was assessed as very low (Table 8).
Hospital-acquired infections increase health care costs through prolonged hospital stays or readmissions.9–11 The direct cost of caring for a patient with an HAI in Canada has been estimated to range from $2,000 to $20,000.12
The outcomes assessed by each study and the definitions used to classify HAIs are summarized in Appendix 3, Table A4. Three of the studies included either infection or colonization with the target organisms as their outcome definition,39,41,43 although one study required that the organism had contributed to increased length of hospital stay.41 Results from these studies were summarized in our results as HAIs, but differences in measured outcomes were noted where applicable. No studies reported on colonization with organisms separately from infection.
Results from this review are in line with prior guidelines set by the National Health Service49 and the Centers for Disease Control and Prevention, 48 which stated that the effectiveness of these devices is yet to be demonstrated and that more research is required.51,52 We note, however, that each of these reviews and guidelines are now outdated; 8 of the 10 studies identified in our review were published in or after 2015.
Uses same data as Nagaraja et al36 with a longer pre- and post-study follow-up period. Data from this study not included in GRADE quality of evidence assessment.
We obtained the costs of UV disinfecting devices from the manufacturers. Obtaining the costs of all commercially available UV disinfecting devices is beyond the scope of the project; we therefore contacted only two leading manufacturers57 (one for xenon devices and one for mercury bulb devices) to obtain cost details. Costs were provided in US dollars (USD). We converted costs into CAD using an exchange rate of 1.325.58 We applied a 5% federal tax for purchasing medical devices and services through a hospital in Canada. A mercury bulb device costs $124,517 CAD ($89,500 USD, including a 1-year warranty) and a xenon bulb device costs $142,325 CAD ($102,300 USD, including a 4-year warranty) (email communications from the manufacturers, Sept 1, 2017, and Sept 14, 2017). The annual warranty ranges between $11,500 to $13,356, which covers the costs of bulb replacement, device parts, and technical support. For the mercury bulb device, there is also a leasing option at a cost of $53,424 per year ($38,400 USD).
Only the study by Levin et al45 commented on deaths attributable to C. difficile, but there were too few deaths to allow for meaningful interpretation. The GRADE for this body of evidence was assessed as very low (Table 12).
At least two portable UV disinfecting products have been approved for sale across Canada (personal communication, Xenex Disinfection Service). This includes the Xenex Light Strike Pulsed Xenon Light Germ Zapping Robot and the Tru-D UVC device, which uses mercury bulbs.
Abbreviations: CLABSI, central line–associated bloodstream infection; CLAUTI, catheter-associated urinary tract infection; GI, gastrointestinal; HAI, hospital-associated infection; MDR, multidrug-resistant; MRSA, methicillin-resistant Staphylococcus aureus; NHSN, National Healthcare Safety Network; SHEA, Society for Healthcare Epidemiology of America; VAP, ventilator-associated pneumonia; VRE, vancomycin-resistant Enterococcus.
What is the published economic evidence for portable ultraviolet (UV) light irradiation as an adjunct to standard environmental cleaning compared with environmental cleaning alone for hospital room surface disinfection?
(cleaning or decontamin* or disinfect* or dis-infect* or terminal or no-touch or non-manual or germicid* or bactericid* or fungicid* or virucid* or bacteriostat*).ti,ab,kf. (1041690)
We are unable to make a firm conclusion about the effectiveness of this technology on HAIs given the very low to low quality of evidence. The budget impact estimates are sensitive to assumptions made about the number of UV disinfecting devices purchased per hospital, frequency of daytime use, and staff time required per use.
Review of the grey literature identified one ongoing study that has potential relevance to this review/research question. The study is titled “Ultra Violet-C Light Evaluation as an Adjunct to Removing Multi-Drug Resistant Organisms (UVCLEAR-MDRO)” and registered in ClinicalTrials.gov. The estimated completion date is March 2018.
Statistically significant reduction (one study) or a non–statistically significant reduction (one study) in C. difficile infection relative rates (very low quality of evidence from two observational studies)
Cost savings related to any potential reduction of HAIs were not included, given our uncertainty about the effectiveness of UV disinfection
Electric polarization
Reduction in Hospital-Acquired MRSA Infection Rates for UV Disinfection Plus Manual Disinfection Versus Manual Disinfection Alone
Direction and magnitude of effect varied across studies, with three studies showing large reduction in infection rates and two studies finding no effect.
Ultraviolet disinfection was primarily used after patient discharge or transfer in nine studies. One study used the device when rooms were vacated for procedures and when operating rooms were cleaned daily.39 One study used the device exclusively for nightly disinfection of operating rooms (Table 1).38
The quality of the body of evidence for each outcome was evaluated according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) framework.34 We started with the assumption that RCTs are high quality, whereas observational studies are low quality. We then rated the studies on the basis of the following considerations: risk of bias, inconsistency, indirectness, imprecision, publication bias, magnitude of effect, and dose-response gradient. The overall quality was determined to be high, moderate, low, or very low using a step-wise, structured methodology. The quality level determination reflects our certainty about the evidence.
Lived experience is a unique source of evidence about the personal impact of a health condition and how that condition is managed, including what it is like to navigate the health care system with that condition, and how technologies might or might not make a difference in people's lives. Information shared from lived experience can also identify gaps or limitations in published research (for example, outcome measures that do not reflect what is important to those with lived experience).63–65 Additionally, lived experience can provide information or perspectives on the ethical and social value implications of technologies and treatments. Because the needs, priorities, preferences, and values of those with lived experience in Ontario are not often adequately explored by published literature, Health Quality Ontario makes an effort to reach out to, and directly speak with, people who live with the health condition, including those who have experience with the intervention in question.
Abbreviations: CI, confidence interval; CLABSI, central line–associated bloodstream infection; CAUTI, catheter-associated urinary tract infection; ESBL, extended-spectrum β-lactamase; MDR, multidrug resistant; SSI, surgical site infection; UV, ultraviolet; VAP, ventilator-associated pneumonia.
Given the limitations of standard manual cleaning and disinfection of hospital rooms for prevention of HAIs, several no-touch ultraviolet (UV) light systems have been developed to supplement current hospital cleaning and disinfection practices.23,24
To fully understand how budget impact varies with different assumptions about parameters, we conducted several sensitivity analyses:
Reduction of individual incidence rates of C. difficile, MRSA, and VRE was not statistically significant when UV was added. However, when all infections were pooled, reduction of incidence rate when UV disinfection was used was statistically significant. See the Clinical Evidence section for more details.
One of five studies evaluated both colonization and infection with C. difficile whereas the other four studies specifically evaluated infection rates. We judge evidence as having no serious indirectness but note variability in hospital settings and patients evaluated as well as measures.
Included study assessed both incident colonization and infection as outcome measure, rather than infection rate alone. But this was already penalized as misclassification of outcome in the risk-of-bias domain.
Many of the included studies looked at feasibility of deployment and reported actual use of the device ranging from 22% to 80% of all eligible discharges.36,41,43–45 In addition to multipatient rooms, reasons cited for not using the device included few devices, communication or notification failures, or urgent need for the room.
Abbreviations: C. difficile, Clostridium difficile; MRSA, methicillin-resistant Staphylococcus aureus; UV, ultraviolet; VRE, vancomycin-resistant Enterococcus.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Unpolarized incident light (natural sunlight, for example) is polarized to a certain degree when it is reflected from an insulating surface like water or a highway. In this case, light waves that have the electric field vectors parallel to the surface are reflected to a greater degree than those with different orientations. The optical properties of the insulating surface determine the exact amount of reflected light that is polarized. Mirrors are not good polarizers, although many transparent materials will be very good polarizers, but only if the incident light angle is within certain limits. In this case, the particular angle inducing maximum polarization is known as the Brewster angle given by the expression:
Outcomes (e.g., outcomes measured, number of participants for each outcome, number of participants missing for each outcome, outcome definition and source of information, unit of measurement, upper and lower limits [for scales], and time points at which the outcome was assessed)
Confidence intervals did not cross no effect; however, confidence intervals were wide in both studies, likely owing to insufficient sample size.
The recommended length of time to run the device varies between devices and manufacturers. The most commonly studied pulsed xenon UV device is developed by Xenex and takes approximately 5 to 15 minutes per run. The entire process of disinfecting a single room is estimated at 15 to 20 minutes.
We searched for studies published from inception of UV disinfection technology to January 23, 2017. We compared portable UV surface-disinfecting devices used together with standard hospital room cleaning and disinfecting versus standard hospital cleaning and disinfecting alone. The primary outcome was HAI from C. difficile. Other outcomes were combined HAIs, colonization (i.e., carrying an infectious agent without exhibiting disease symptoms), and the HAI-associated mortality rate. We used Grading of Recommendations Assessment, Development, and Evaluation (GRADE) to rate the quality of evidence of included studies. We also performed a 5-year budget impact analysis from the hospital's perspective. This assessment was limited to portable devices and did not examine wall mounted devices, which are used in some hospitals.
Polarization oflight
Risk of Biasa Among Uncontrolled Before-After Studies for Comparison of UV-C Disinfection as Adjunct to Manual Cleaning and Disinfection Versus Manual Cleaning and Disinfection
(((Health care* or healthcare*) adj2 (acquired or associated) adj2 (infection* or disease* or pathogen*1)) or (cross adj2 (infection* or disease* or pathogen*1)) or HAI or HAIs or HCAI or HCAIs or nosocomial*).ti,ab,kf. (89022)
The RCT reported the combined reduction in infection and colonization, but did not report the reduction in infection or colonization separately. Given colonization and infection have very different costs and outcomes, results reported by the RCT could not be used without making a variety of assumptions.
(((Health care* or healthcare*) adj2 (acquired or associated) adj2 (infection* or disease* or pathogen*1)) or (cross adj2 (infection* or disease* or pathogen*1)) or HAI or HAIs or HCAI or HCAIs or nosocomial*).ti,ab,kf. (89022)
We estimated the labour cost of operating UV devices by multiplying the time required from a hospital staff member by the hourly cost of labour (Table 14). The cost of labour includes wages paid to employees, as well as the cost of employee benefits and payroll taxes paid by an employer. The cost of a hospital environmental service (EVS) worker is estimated to be $28.60 per hour ($22 for the hourly wage59 plus 30% employee benefits60).
Despite best practice recommendations, how manual cleaning and disinfection is performed in Ontario hospitals varies (expert communication, Dec 2016).20 Evidence also suggests that manual cleaning and disinfection may be suboptimal, resulting in residual contamination.21 Additionally, manual cleaning and disinfection protocols can be complex and require disinfectants that are fast, broad spectrum, safe for humans and the environment, but also compatible with materials and medical devices.22 Adequate disinfection also requires tailoring the method of disinfection to the microorganisms being targeted, such as the use of sporicidal agents (e.g., sodium hypochlorite [bleach]) to inactivate spore-forming bacteria like C. difficile. In addition to the type of disinfectant used, effective disinfection requires appropriate application, which includes adequate cleaning prior to application, sufficient contact time between the disinfectant and the surface being cleaned, and appropriate concentrations of disinfectant used, all of which can be difficult to achieve.22
Devices emitting UV light are no-touch, automated disinfection systems that are used to kill pathogens associated with infectious disease and infections.25 These devices work primarily through the use of lamps that produce high-intensity ultraviolet C (UV-C) light, a form of electromagnetic radiation (UV-C wavelengths of 100–280 nm on the electromagnetic spectrum). UV-C is germicidal; it destroys the DNA of bacteria, viruses, and other microorganisms, preventing them from multiplying, repairing the damaged DNA, and causing infections and disease.26 Ultraviolet surface-disinfecting devices are not intended to replace other environmental cleaning practices, but rather to be used as a complementary method to enhance disinfection after surfaces are manually cleaned and disinfected.
Pathogens that cause HAIs can be transmitted from one patient to another through direct or indirect contact. While person-to-person touch is an important mode of transmission, contaminated surfaces in health care settings can contribute to the transmission of microorganisms implicated in HAIs.13–15 Bacteria can thrive on many objects, such as bed rails, call buttons, telephones, door handles, mattresses, taps, bathroom fixtures, and chairs. Bacteria and viruses can survive on these surfaces for long periods, with C. difficile spores surviving in the health care environment for up to 5 months, and MRSA and VRE surviving on dry surfaces for several weeks to months.16
Three studies evaluated the use of mercury UV-C devices (one cluster RCT, one time-series analysis with a control group, and one uncontrolled before-after study). Each of the mercury UV-C studies used a device by a different manufacturer (Tru-D, Optimum-UV Clorox Healthcare, or IRiS 3200m) (Table 1). The remaining seven studies evaluated pulsed xenon UV devices using an uncontrolled before-after study design. Six of these studies used the Xenex device and one did not state the specific device or manufacturer used.
A key component of health technology assessment is the clinical review, which carefully analyzes all clinical outcomes. Patient engagement can often provide context for which patient outcomes are most important and relevant to a patient population. In this health technology assessment, however, patient-relevant outcomes were expected to match outcomes deemed important by clinicians with a high degree of correlation. For this particular health technology assessment, it was thought that patients were most likely to desire a successfully disinfected room, to prevent the spread of hospital infections. We believe this desire would closely align with the outcome desired by clinicians and administrators implementing UV disinfection.
On the basis of very low to low quality of evidence, we are uncertain whether the use of portable ultraviolet light (UV) disinfecting devices as an adjunct to standard hospital cleaning and disinfection further reduces hospital-acquired infections.
GRADE Evidence Profile for Hospital-Acquired C. Difficile Infection–Related Mortality Rate, Comparison of Pulsed Xenon UV Devices Plus Standard Disinfection Versus Standard Disinfection Alone
Decontamination of patient rooms through cleaning and disinfection is a key method for comprehensive infection prevention and control and is critical in reducing and preventing the transmission of pathogens in the health care environment.18 Cleaning is defined by the physical removal of foreign material or surface debris, while disinfection refers to killing or inactivation of microorganisms that can cause infection.18
When current is applied to the electrodes, the liquid crystalline phase aligns with the current and loses the cholesteric spiral pattern. Light passing through a charged electrode is not twisted and is blocked by polarizer 2. By coordinating the voltage on the seven positive and negative electrodes, the display is capable of rendering the numbers 0 through 9. In this example the upper right and lower left electrodes are charged and block light passing through them, allowing formation of the number "2".
Hospital-acquired infections are infections that patients develop while in the hospital that were neither present nor developing when patients were admitted. In Canada about 10% of adults with short-term hospitalization have hospital-acquired infections. We studied the effectiveness and budget impact of portable ultraviolet light surface-disinfecting devices for reducing hospital-acquired infections.
Results of the sensitivity analyses are presented in the Tornado diagram (Figure 3: Tornado Diagram Evaluating Influence of Key Parameters on Net Budget Impact). The net budget impact was most sensitive to the number of devices purchased by the hospital, frequency of use during daytime, and staff time required per use. Four factors had a moderate impact on the results: assumption regarding nighttime usage of the UV devices, leasing the devices instead of buying (mercury bulb device only), assumption regarding whether staff can perform other tasks during the UV cycle (xenon bulb device only), and cost of the UV device. Results were not sensitive to assumptions regarding who operates the UV devices (any EVS worker vs. a dedicated operator).
Hospital-acquired infections can be caused by a range of microorganisms including bacteria, viruses, or fungi that are present in the hospital environment. The most commonly monitored HAIs in Canada include Clostridium difficile, methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus (VRE), and carbapenemase-producing Enterobacteriaceae (CPE).3–5 These HAIs can result in serious illness and sometimes death, with longer hospital stays and readmission.6 As such, HAIs are considered a serious adverse outcome in the delivery of care to patients across the health care system.
Numerous UV room disinfecting devices have entered the North American market. The current use and dissemination of UV disinfecting devices in Ontario remains unclear. According to experts, several devices have used or are being used in Ontario hospitals, although dissemination has been slow (expert consultation, December 2016).
The RCT by Anderson et al43 did not find a relative reduction in combined hospital-acquired VRE infection and colonization rates among patients exposed to seed rooms that were disinfected with mercury UV-C devices compared with standard manual disinfection alone—although the results were statistically underpowered (Table 9). This body of evidence was assessed as low quality (Table 10).
With a xenon bulb device, a total of 18 minutes is required per room (three 5-minute cycles at different locations plus 2–3 minutes for positioning for patient rooms42,62; or two 8- or 10-minute cycles for operating rooms38,55). Because the device requires multiple cycles/positions, an operator needs to stay nearby and move the device to a new location every 5 minutes. In the base case, we assumed that an EVS worker can perform other tasks (e.g., clean the bathroom) during this 5-minute interval. For sensitivity analysis, we assumed that 5 minutes is too short to allow staff to perform other duties.
We included studies of portable UV surface-disinfecting devices used as an adjunct to standard hospital room cleaning and disinfection. Both pulsed xenon disinfecting devices and mercury bulb UV-C devices were included.
In sensitivity analysis, we assumed that a dedicated UV device user/operator would be needed, as this was the experience of some Canadian hospitals. According to Spencer et al61 at Vancouver General Hospital, where UV devices were pilot tested, EVS workers would manually clean a room and enter the completed job into a computer, which would generate a call to the dedicated UV device operator. This system not only allows EVS workers to continue with the next job, but also enables the UV operator who understands the overall cleaning needs of the hospital to prioritize areas with the most opportunity to improve their HAI rates. This system could be especially helpful when multiple areas in a hospital need to be cleaned with UV devices at the same time.
Both studies evaluating the use of pulsed xenon UV devices were adequately powered but had several other limitations. Both studies found a relative rate reduction in hospital-acquired VRE rates when the UV device was added to manual cleaning and disinfection (18%–50% reduction in relative rate) (Table 9). The GRADE for this body of evidence was assessed as very low (Table 10).
In Ontario, C. difficile constitutes the largest proportion of HAI (expert consultation, May 2017). For this reason, we decided to focus primarily on C. difficile in this review.
(((health or healthcare or care or medical) adj2 (facility or facilities or center* or centre* or setting* or institution*1)) or hospital*1 or ((healthcare or health care) adj environment*1) or (room*1 adj2 (patient* or private or semi-private or semiprivate or recovery or isolation)) or ward or wards or ((intensive or critical) adj2 unit*) or ICU or ICUs or acute care).ti,ab,kf. (2972961)
Included study assessed both incident colonization and infection as outcome measure, rather than infection rate alone. This was not considered to be a serious source of indirectness.
Among the six studies evaluating the use of pulsed xenon UV devices (Table 3), two studies (Haas et al35 and Nagaraja et al36) used the same hospital dataset with various follow-up periods and subgroups. Given Nagaraja et al36 focused only on C. difficile rates and published most recently, only total results from this study were used in the GRADE quality of evidence assessment.
130 Bloor Street West, 10th Floor, Toronto, Ontario, M5S 1N5, Tel: 416-323-6868, Toll Free: 1-866-623-6868, Fax: 416-323-9261, Email: EvidenceInfo@hqontario.ca, www.hqontario.ca
In addition to a standard manual cleaning arm (bleach for C. difficile discharge and quaternary ammonium for all discharges), the cluster RCT by Anderson et al43 evaluated four enhanced cleaning study arms: UV alone, UV plus usual manual cleaning, bleach alone, and bleach plus UV. Given comparisons between the bleach alone and bleach plus UV disinfection arms were not adjusted, results for only the usual manual cleaning arm and the usual manual cleaning plus UV arm were included in our review.
(((health or healthcare or care or medical) adj2 (facility or facilities or center* or centre* or setting* or institution*1)) or hospital*1 or ((healthcare or health care) adj environment*1) or (room*1 adj2 (patient* or private or semi-private or semiprivate or recovery or isolation)) or ward or wards or ((intensive or critical) adj2 unit*) or ICU or ICUs or acute care).tw,kw. (2988778)
The 5-year budget impact for using pulsed xenon UV devices was slightly lower than mercury-based technology if we assume that two devices would be purchased per hospital. However, this comparison is sensitive to the number of devices purchased per hospital, daytime frequency of use, and staff time required per use.
Anderson et al43 conducted the first randomized controlled trial (RCT) to evaluate the effect of enhanced room disinfection after patient discharge or transfer on HAIs from multidrug-resistant organisms. The researchers compared three enhanced strategies (UV plus quaternary ammonium, UV plus bleach, and bleach alone) with quaternary ammonium. Several characteristics of this study limit the data's usefulness for an economic evaluation:
Five studies reported on hospital-acquired MRSA infection rates (two evaluated mercury UV-C devices and three evaluated pulsed xenon UV devices) (Table 7). Overall baseline rates of hospital-acquired MRSA infection ranged from 0.34 per 1,000 patient days to 5.03 per 1,000 patient days.
Several observational studies reported using UV disinfecting devices could lead to cost savings by reducing the number of infections. Fornwalt et al55 estimated $290,990 in potential savings from prevention of seven surgical site infections and one death during a 12-month period, at $20,785 per infection. Miller et al40 stated that $300,000 would be saved by avoiding 29 Clostridium difficile infections during a 15-month period, at $13,500 per case. Catalanotti et al38 estimated $478,055 would be saved by preventing 23 potential Class I surgical site infections and one death during a 21-month period, at $20,785 per infection. However, these estimates are very crude and do not take into account the cost of acquiring and operating UV disinfecting devices.
(((multidrug or multi-drug or antibiotic* or antimicrobial) adj (resistance or resistant)) or MDRO or MDROs or ARO or AROs).ti,ab,kf. (188047)
Clinical relevance of this study is limited for several reasons. First, the authors combined both infection and colonization with target organisms as their outcome measure. It was noted that 54% of all outcomes reported were infection, but no data stratified by infection alone could be obtained. Combining both infection and colonization likely improved statistical power, but it remains uncertain whether impact on HAIs alone would be clinically relevant. Because only a small proportion of C. difficile or multidrug-resistant organism colonizations lead to eventual infection,46–49 the clinical impact on outcomes such as morbidity, mortality, and excess length of stay are more difficult to ascertain. Second, the study evaluated infections only among patients admitted to rooms previously occupied by patients with infection or colonization with one or more target organisms. While providing valuable information on the spread of organisms to subsequent patients admitted to the target room, the effect of room disinfection after patient discharge or transfer on hospital-wide infections through other forms of indirect contact was not reported. Study authors stated that secondary analyses evaluating incidence of hospital-wide target organisms will be presented elsewhere; however, these data are currently unpublished.
(((Health care* or healthcare*) adj2 (acquired or associated) adj2 (infection* or disease* or pathogen*1)) or (cross adj2 (infection* or disease* or pathogen*1)) or HAI or HAIs or HCAI or HCAIs or nosocomial*).tw,kw. (91671)
No reduction in MRSA (one study) or non–statistically significant reduction in VRE (one study) relative rates (very low quality of evidence from two observational studies)
Included study assessed both incident colonization and infection as outcome measure, rather than infection rate alone. But this was already penalized as misclassification of outcome in the Risk of Bias domain.
The core protocol is to place the device in vacant patient rooms, running it once in the bathroom and once on each side of the hospital bed (personal communication, Xenex Disinfection Service, Feb 2017). Surfaces must be in the line of sight to be decontaminated, and disinfection is therefore limited by shadowed areas and depends on the reflectivity of room walls and surfaces. The amount of UV-C light reaching organisms and the effectiveness of the light is dependent on the dose and intensity, the distance from the object being disinfected, the type of surfaces, and the type of microorganisms present.28 Rooms are vacated and doors are closed during the disinfection process, and devices must be built with sensors that automatically stop the irradiation if the door is opened or any other movement is detected. Some manufacturers offer a protective curtain, which can be placed between patient beds to allow for partial disinfection of shared patient rooms (personal communication, Xenex Disinfection Service, Feb 2017).
Two of the identified studies used the same dataset for their analyses; however, both were included in the review because different comparisons and subgroups were evaluated.35,36 The most recent study was used in the GRADE assessment when the same outcome was assessed.
The statements, conclusions, and views expressed in this report do not necessarily represent the views of the consulted experts.
Reduction in Other Hospital-Acquired Infection Rates for UV Disinfection Plus Manual Disinfection Versus Manual Disinfection Alone
To complete the needs assessment, background reading into the topic of UV disinfection included reading the clinical review plan and consulting clinical experts in the field. A qualitative literature scan was also conducted.
Throughout development of this analysis, we solicited advice from clinicians with expertise in HAI prevention and control or in using UV disinfecting devices in a hospital. The role of expert advisors was to review the structure and inputs of the economic analysis to confirm that the information we used reasonably reflects the clinical setting.
There are two main types of portable UV devices for surface disinfection that have been approved for sale in Canada: those that emit a continuous dose of UV-C light through a mercury bulb, and those that use a pulsed xenon light.25
A single reviewer reviewed titles and abstracts and, for those studies likely meeting the inclusion criteria, we obtained full-text articles.
The RCT by Anderson et al43 found no cases of multidrug-resistant Acinetobacter infection or colonization among patients exposed to seed rooms with or without the use of UV disinfection.
After careful consideration of these factors within the needs assessment, the patient engagement team concluded that that direct patient engagement would provide minimal value to and impact on this health technology assessment.
What is the effectiveness of portable ultraviolet (UV) light surface-disinfecting devices as an adjunct to standard cleaning and disinfection protocols in reducing hospital-acquired infections versus standard cleaning and disinfection protocols alone?
The target setting for UV disinfecting devices is hospitals. Devices might be used in several places, including contact precaution rooms after patients are discharged, intensive care units (ICUs), other medical/surgical wards, and operating rooms where HAIs are more likely to occur.




 Ms.Cici
Ms.Cici 
 8618319014500
8618319014500