LED Bright Spotlights - high power spot light
We conclude that microscope preferences can only be used to predict display luminance requirements where the microscope is being used at very high brightness levels. A display capable of a brightness of 500 cd/m2 should be suitable for almost all pathologists with 300 cd/m2 suitable for the majority. Although display luminance is not frequently changed by users, the ability to do so was felt to be important by the majority of respondents.
In contrast to radiology, current pathology practice does not involve the regulation of ambient lighting and in the UK consultants generally work in individual use offices where further variation in ambient light is introduced by individual preference.10,17 This makes sense given that the closed nature of a microscope is far less likely to be impacted by ambient lighting. Furthermore, microscopes allow the user to make easy adjustments to the lighting by a continuous dial which allows for adjustment for individual sensitivities to light as well as to navigate tissue factors such as thick sections. Anecdotally, there is significant variation between pathologists in their use of microscope brightness levels, perhaps especially noticed by trainee pathologists who are more likely to use double-header microscopes to review images and to rotate between a number of microscopes, left at the setting of the previous user, during their training. Deploying digital pathology systems in such variable ambient conditions and for pathologists who are used to sensitive and easy control of light while they work presents an additional challenge for departments in setting up displays.
A scripted protocol was used from the consent process through to completion of the experiment to standardize data collection.
A convenience subsample of respondents was then invited to take part in a practical task to determine microscope brightness and display luminance preferences in the normal working environment. A novel adaptation for a lightmeter was developed to directly measure the light output from the microscope eyepiece.
2 waysto adjust lighton microscope
Our focus was creating a tool which was able to reliably discriminate between fine increments of light adjustment at the microscope for intra- and interpathologist comparisons and cross-modality correlations, rather than achieving true accuracy of light measurement. The final iteration of this development process is pictured in supplementary Fig. A1 alongside images of design and the tool in use.
David Brettle reports a relationship with Jusha Commercial & Trading Co, Ltd. that includes: consulting or advisory. If there are other authors, they declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
The reporting environment of light preference task participants. For participants of the light preference task, measurements of the ambient lighting (A) and of their reporting display position (B) at the time of the experiment were captured. Icons provide a visual reference of the display positions described and are further described as follows; “Side on” where display is viewed at 90° to natural light; “Side-facing” where display is viewed at 45° to natural light; “Facing” where the natural light is behind the pathologist 180°; “In front” where the natural light is behind the display 0°.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
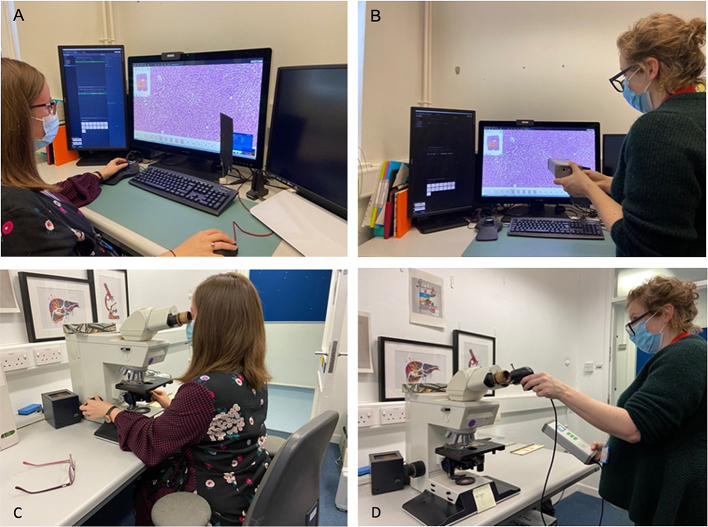
An LXCan spot luminance meter (IBA international, Louvain-La-Neuve, Belgium. Within manufacturer calibration at the time of use) was used to measure ambient lighting/illuminance (lux) and display luminance (cd/m2). Light output directly from the microscope eyepiece was also measured using the illuminance detector via the development of a novel adaptation (described in Appendix). Slides of two different tissue types (breast and liver) were prepared in the departments own laboratory following usual hematoxylin and eosin staining protocols and converted to digital images on an AperioGT450 scanner (Leica Biosystems, Nußloch Germany), the scanner normally used in the department. Corresponding areas on the slides and images were marked to direct the pathologists to a specific region of the tissue and control at what magnification it would be assessed (Fig. 1).
The lack of correlation between microscope and display preference means microscope preference cannot be used to guide display setup, except perhaps where users have a very bright microscope preference as this was better correlated with a brighter display preference. Lack of correlation may relate to differences in what users are trying to achieve with light adjustment on each modality, as highlighted by our survey results in which microscope adjustments were predominantly for slide factors, whereas for the display adjustments for environmental lighting and visual comfort were more common.
Corresponding author at: NPIC Centre, Level 2, Sir Robert Ogden Building, St James's Hospital, Beckett Street, Leeds LS9 7TF, UK. charlotte.jennings1@nhs.net
National Pathology Imaging Co-operative, NPIC (Project no. 104687) is supported by a £50 m investment from the Data to Early Diagnosis and Precision Medicine strand of the government's Industrial Strategy Challenge Fund, managed and delivered by UK Research and Innovation (UKRI).
Raw results from both the online survey and practical light preference assessment can be made available on request from corresponding author CJ.
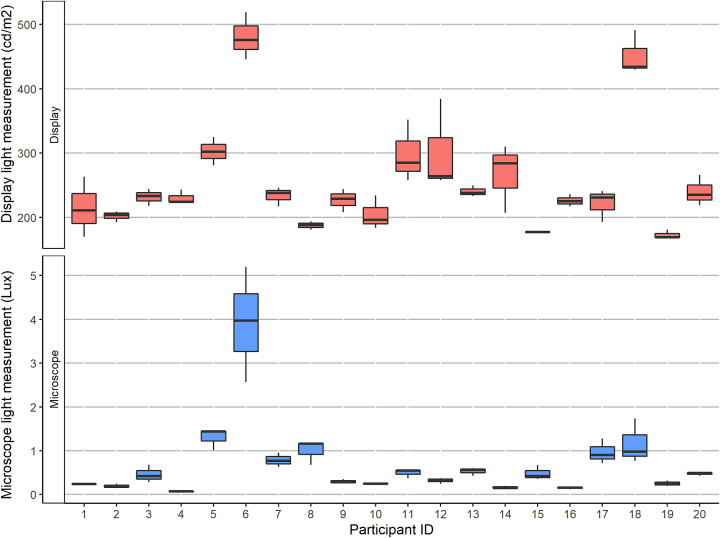
Microscope light preferences ranged from 0.06 to 5.2 lx, representing nearly a 100-fold difference in preference. Pathologists generally had quite narrow preference ranges on the microscope (16/20 had interquartile range < 0.5 lx), but a few exhibited a much broader range (P6; interquartile range 2.6 lx) (Fig. 8).
Platform that supports a microscope slide
In comparison, only 11% reported ever adjusting the backlight settings on their digital display. Of those that had adjusted their displays (n=7), the frequency spectrum of adjustments was just as broad, and one user also indicated they adjusted the display for every case (possible respondent error).
There was marked variation in the ambient lighting between different participant's offices (range 39–1308 lx), however the majority were operating in normal “office” conditions of around 300 lx. Options for lighting adjustment within different offices was variable, including access to and use of blinds, additional lighting (e.g. uplight lamps and desk lamps) and number and position of overhead bulbs. All participants had offices with an external facing window. Display equipment was mostly positioned “side-on” to windows, where this was not the case this was largely dictated by room layout (Fig. 7).
Twenty consultants took part in the practical brightness assessment. Light preferences on the microscope showed no correlation with display preferences, except where a pathologist has a markedly brighter microscope light preference. All of the preferences in this cohort were for a display luminance of <500 cd/m2, with 90% preferring 350 cd/m2 or less. There was no correlation between these preferences and the ambient lighting in the room.
Development of the lightmeter adaptor. (A) CAD design of the integrating light sphere; (B) Images of the final integrating light sphere adapter; (C) Integrating light sphere in use, connecting to the microscope eyepiece and LXCan Spot luminance meter to measure the light output directly from the microscope.
For most participants, the experiment preference represented minimal change from their “pre-experiment” settings. However, for others, the experiment highlighted a noticeable difference (Fig. 9). This is supported by the results of the survey cohort which also indicated that most users are happy with their current display luminance.
The survey (response rate 59% n=64) indicates 81% of respondents adjust the brightness on their microscope. In comparison, only 11% report adjusting their digital display. Display adjustments were more likely to be for visual comfort and ambient light compensation rather than for tissue factors, common for microscope adjustments. Part of this discrepancy relates to lack of knowledge of how to adjust displays and lack of guidance on whether this is safe; But, 66% felt that the ability to adjust the light on the display was important.
A number of the participants made comments that they felt their preference would vary on different days for a number of reasons such as tiredness or room lighting. It was also noted by a few that their tolerated range at the display was probably quite broad and that a diagnostically acceptable range may be broader still.
We also recognize that display and image management system software settings for brightness, contrast and color profile may all have an impact on image perception. Here, we have focused on light intensity and have not assessed other parameters available outside the recommended settings of the display manufacturer. We appreciate there is more nuance to image perception overall and this probably underlies the lack of correlation found between modalities in our work. Yet, we found convincing personal preferences indicating that light intensity is a relevant variable to consider. Further work may elucidate the relationship between these factors.
Survey participant reasons for light adjustment when reporting at the microscope or digitally. Pathologists in the survey cohort who indicated they did adjust the light sometimes; microscope (n=52) and digital (n=7) provided reasons for this by selecting from categories provided or by indicating “other” and adding a free-text response. Participants were able to select multiple options to best reflect their light use habits.
An opportunistic sample of 20 consultants took part in the practical light adjustment task, representing 50% of the target cohort. Due to the anonymous nature of the survey, the overlap between participants in this cohort and those who completed the survey is unknown. Although not explicitly collected as part of the study, comments from participants were used to infer usage and experience with digital pathology as follows; primary reporting with digital pathology (n=7), secondary uses only, e.g. teaching/training, multidicisplinary team meeting reviews (n=7), and minimal or no digital pathology use (n=6).
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
All statistics and graphical figures created within R computing environment: RStudio Version 2022.02.0 © 2009–2022 RStudio, PBC. “Prairie Trillium” for Windows. R version 4.2.1 (2022-06-23 ucrt) – “Funny-Looking Kid” Copyright (C) 2022 The R Foundation for Statistical Computing Platform: x86_64-w64-mingw32/x64 (64-bit). Additionally installed packages on top of the Base R (4.2.1) including:gtsummary, ggpubr, dplyr, cowplot, dplyr, ggplot2, naniar, readr, reshape2, stats and tidyr.
The online survey was completed by 64 pathologists, a response rate of 59%. The respondents included 52 consultants (65%) and 12 trainees (43%) and covered the full working age range of the cohort (Fig. 3). A variety of different work patterns were represented, with participants spending between 1 and 63.5 hr reporting per week.
Images of the experiment set up for the light preference task. Assessment (A) and measurement (B) on the digital display and assessment (C) and measurement (D) at the microscope of light preferences when viewing a whole-slide image. The experiment was conducted in pathologists' own offices and on their usual reporting equipment. Preference was defined for participants as “a point where you feel visually comfortable and also feel able to assess features of the slide or image at a level that is needed for reporting”. Pathologists were not asked to give a diagnostic assessment of the slides/images provided.
A real-world approach was used in the light preference task, accepting lack of control for several variables such as environment lighting, equipment positioning, type of bulb and use of light filters on microscopes, and testing at different times of the day or week. Participants were asked to replicate their usual reporting setup, with consideration to their environment, equipment, and selves, which we felt suited our research aim of being better able to set up users for digital pathology in our department. However, further work which addresses the impact of these parameters may help to define optimal working conditions for digital pathologists. Similarly, it would be valuable to understand how light use and preference changes during a prolonged period of reporting rather than the snapshot we have captured here. As supported by our survey, visual comfort is a common precipitant of light adjustment across both modalities and this becomes more relevant over time, where accommodation and visual fatigue are more apparent.29
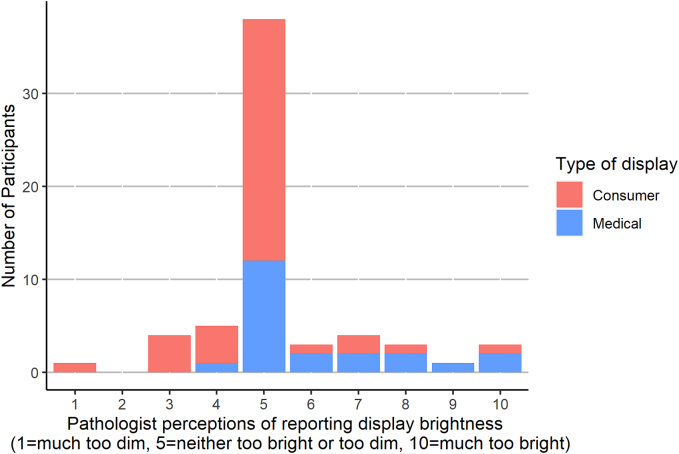
The majority of respondents (59%) found their displays “neither too bright or too dim” for viewing digital images. Outside the majority, a relatively even spectrum existed of those who found the display too bright or too dim to some degree. The survey cohort included those who had high specification medical grade displays as well as those with consumer grade displays (Fig. 6).
But learning from experience in radiology, guidelines will be necessary to ensure that the technical performance of these displays is sufficient as well as to address ergonomic aspects of display working.8,10, 11, 12
The overall strength of opinion from the survey cohort on the importance of light adjustment on both modalities indicates that this is a function that may need to be addressed in digital display development. Whilst the number who adjust their display light settings was small (n=7), a range of frequency of adjustments was represented in this sample. Current displays are far less easy than a microscope to adjust. Unfortunately, the level of knowledge about how to adjust display settings and the confidence level in doing so in this cohort was not captured as part of the study. However, comments provided by survey participants did indicate that this was an issue for some.
Additional eyepieces (commonly used for training to allow side by side reporting) or cameras (used to photograph a specimen) can be inserted before the main eyepiece and involve the use of additional lenses to direct the image forming rays and the illuminating rays. In our department, there are many different microscopes—variable in their make, model and age. While most consultants have an attachment to allow double-headed viewing, trainees usually do not. A minority of the consultants also have a camera attachment. This means that the light intensity of the bulb in the base of the diaphragm (which could be measured from the collector lens) is variably representative of the light intensity at the eye piece. For this reason, we wanted to devise a method to measure the light output from the eyepiece directly. In a review of the literature, we could not find any examples of others having measured this before.
Finally, whilst we strongly feel there is a need to define critical performance parameters of these digital pathology displays, this work shows that individuals, their preferences and their working habits need to be considered in the process.
Display luminance preferences on the digital display ranged from 169 to 519 cd/m2, representing a more limited inter-pathologist variation than seen at the microscope. However, a similar pattern was observed whereby some participants had relatively narrow interobserver variability for preference (P8; interquartile range 13 cd/m2) and others showed less distinct preference (P12; interquartile range 384 cd/m2). This finding was supported by comments of a few participants during the display part of the experiment who felt that they would be happy at a range of light levels on their displays and found it harder to define their preference point.
Demographic factors of survey participants. Participants (n=64) are split by their role and age (A), and by the number of hours spent reporting per week (B). Reporting hours are broken down into time spend on each reporting modality (microscope or digital).
In 2018, our pathology department (Leeds Teaching Hospitals NHS Trust, UK) implemented 100% digital scanning of all slides. As part of this process, consultant pathologists were supplied with large, medical-grade, high resolution and high luminance displays which were chosen based on best available evidence (Jusha, Nanjing Jusha & Commercial Trading Ltd., China: Model C620L with 6 megapixel 30-in. display and luminance up to 800 cd/m2), as summarized in the Leeds Guide to Digital Pathology Vol 1.14,15 A minority of users struggled with the perceived “brightness” of these displays and were developing symptoms of visual strain. In attempting to tailor the display to these users as per Government Health and Safety Display Screen Equipment guidance, a conflict arose in altering the medical-grade monitor from its approved settings.16 Similar conflicts between display parameters and visual strain were experienced in radiology and have largely been navigated through ambient light control and ergonomic working practices and have again been incorporated into guidance documents.10
It was possible to separate the cohort of respondents with high specification medical grade displays. The majority of this cohort (54%) also found their display “neither too bright or too dim” but those outside of this were more likely to find their display too bright to some degree.
This uncertainty is reflected in the approach taken by the US Food and Drugs Administration (FDA) to grant clinical approval to a whole system, with a pre-defined display.13 However, during the COVID pandemic, the drive to enable remote working (on different displays) was met with a statement from the FDA that pathologists should “use their clinical judgement to determine whether the quality of the images…are sufficient for interpretation” and indicates a move towards pathologists having a responsibility to ensure their displays are fit for purpose, as they do for their microscopes.6
Using average preference values for display luminance, 70% of pathologists prefer a display luminance of 250 cd/m2 or less, 85% 300 cd/m2 or less and 100% 500 cd/m2 or less.
The light preference task was conducted in consultants' offices, where there was variation in ambient light levels, but surprisingly display preferences were not correlated to ambient light (correlation coefficient of 0.27). Several studies in radiology have demonstrated ambient light has an impact on performance.21, 22, 23 Such studies led to control of ambient light in reporting environments of radiologists to achieve sufficient contrast detection without inducing visual strain from display use at high luminosity.11 We did not undertake diagnostic performance measures as part of this work and further assessment is needed to understand the relationship between preference and performance in pathology. The practicality of low ambient light working for pathologists seems limited until the whole workflow is digital given the number of other tasks pathologists undertake when reporting but should be considered as an option to achieve visual comfort for those with lower light preferences or who are experiencing visual strain.18 Current pathology workspaces should also be altered to optimize display position relative to bright light sources such as windows, as this has been shown to reduce performance in a pathology specific contrast performance task, with the optimal position being side-on to a window.24 However, alterations may not be possible in all cases. In this study, some pathologists were limited in adjusting their equipment layout by room constraints and to ambient light levels by the absence of blinds.
Brightness adjustment microscope
Adjustment of light at the microscope was common, with 81% of our respondents adjusting the light on some occasions. The frequency of light adjustment covered the full spectrum of the scale that was presented [1=never, 5=half of reporting sessions, 10=every case]. Most of the participants (73%) estimate adjusting microscope light settings half of the times they report or less. However, one respondent reported making light adjustments for every case they view (Fig. 4).
Pathologists' light preferences at the microscope (A) and digital display (B). Preferences when viewing the “test” slide of breast tumor tissue recoded at each reporting modality. P6 and P18 were outliers with notably higher display preferences and correspondingly high microscope preferences as discussed in the text.
Raw results from both the online survey and practical light preference assessment can be made available on request from corresponding author CJ.
Adoption of new technologies is linked with perceived ease of use and in this situation, it may be achieved by offering an experience that is familiar and as easy as microscope light adjustments.25 Display development in other areas has sought to use this principle and shown increased speed and comfort with digital pathology when image viewing software captures the feel of microscope slide review.26,27 These results may therefore be of interest to display developers and manufacturers. Facilitating preference needs to be balanced against performance and technical image parameters may need to be defined within which users can make fast, “eyes free” adjustments as they work.
CJ, DT and DB conceived and planned the study. CJ carried out the experiments and data acquisition. CJ and DB analyzed the data and CJ wrote the manuscript, which was revised by DT and DB. The final version has been approved by all authors.
Comparison of pre-experiment display luminance and experiment display preference in light preference cohort. The pre-experiment measured screen luminance compared with mean preference measurement during the experiment for each participant of the light preference task.
Controlled experiment views on display and microscope. Marked up (pen) area of slide (A) and marked up image (B) of the section of liver parenchyma used in demonstration of the practical task. Pathologists were advised to center their view at the middle of the markings and increase the objective lens until the marking was just out of view (microscope) or the digital magnification until the green box was at the edge of the display (display). This set the viewing magnification on both modalities at 20× (C and D). The “microscope” image above was captured digitally to enable easier comparison of the two methods used. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Participants were able to select multiple options to describe the reasons for light adjustment on their equipment. The options given included adjustments for slide-related features (such as for specific diagnostic features, specific stains or tissue types and slide quality issues), viewing at different objectives, changes in environment lighting, for visual comfort or adjustment from another user. All users who adjust their lighting do so for multifactorial reasons. For those who adjust their digital display, visual comfort and changes in environment lighting are the dominant factors. In contrast, at the microscope, slide factors predominate (Fig. 5).
A number of general comments were given to support the importance of adjusting light which covered both reporting factors and user factors, examples in Table 2.
Survey pathologist perceptions of their reporting display brightness. All survey participants rated their reporting display for brightness according to a scale of 1=“much too dim”, 5=neither too dim or too bright and 10=“much too bright”. Consultant pathologists at one center had high-grade “medical” displays (n=22) whilst all other pathologists had “consumer” grade displays (n=42) and the pathologist display rating has been split above according to these categories.
Lightswitch microscope function
The same approach was taken on the microscope, taking a pre-experiment measurement, working through a demonstration slide (liver parenchyma) and then repeating three times on the test slide (breast tissue). On the microscope, the experiment controller reduced the microscope light dial to its minimum before the experiment began but the participants were invited to control the dial when choosing their preference. Experiment setup pictured in Fig. 2.
which of the three factors affecting image quality is altered by thelightsource?
The light preference task took place in large pathology department with established digital pathology workflows and good exposure to digital pathology, however use of digital pathology for primary reporting in this cohort was variable and was not captured in our results, except where users made comments specifically relating to their experience. Less-experienced users may have found identifying their preference on this modality more challenging and thus, it may be a less accurate reflection of the variation of preference. Other participant demographics, such as age and ocular health may be of interest for future work with a larger sample size.
Thank you to all the participating pathologists across the West Yorkshire Association of Acute Trusts Region who generously contributed their time in completing the survey and/or practical assessment.
The experiment entailed a light preference adjustment task performed on slides and digital images in the participants usual workspace on their usual reporting equipment. Preference was defined for participants as “a point where you feel visually comfortable and also feel able to assess features of the slide or image at a level that is needed for reporting”. Pathologists were not asked to give a diagnostic assessment of the slides/images provided. One-to-one appointments were made with author CJ to conduct the experiment. The appointments were to fit with pathologist availability and varied throughout the day over the 2-month period of the study.
Further work needs to be undertaken to establish the relationship between diagnostic performance, luminance preferences, and ambient lighting levels.
The survey was conducted through Microsoft Forms and shared via email to a lead pathologist at each trust who circulated the survey to their teams. The survey was composed of 12 questions and captured limited demographic data, such as age and role, as well as information about light use habits on microscope and display. General opinions about the importance of light adjustability were also invited in a free-text question. Three reminder emails were sent over a period of 8 weeks before the online form was closed to further responses. A copy of this questionnaire is available for review in Supplementary materials.
Concentrateslightonto the specimen
Some of the pathologists in our survey were less sure about how light use would impact reporting digitally, highlighting a lack of knowledge of displays in general as well as inexperience in digital pathology—a knowledge gap also recently described by Abel et al.6 The need to adjust for ambient lighting and visual comfort is a sufficient argument for this function in the “new microscope” but it was useful to capture the thoughts of more experienced digital pathology users who similarly to at the microscope find that short-term light adjustments can help identify specific features such as mitoses more easily. The development of clear guidance and education on displays and their functions will be needed to provide pathologists with confidence in the use and adjustment of their reporting equipment, especially if pathologists are to be responsible for it as recent FDA guidance suggests.6 The development of tools such as the Point of Use Quality Assurance tool (a free online tool in which users check their performance in contrast detection test) can support pathologists to assess their own working environment.28
A few respondents with no digital pathology experience felt less able to comment on the importance of light adjustment on this modality, for example “I don't report diagnostic digital slides so I am unsure whether I would use the digital slides in the same way”. However, others felt light adjustment was a core part of reporting “I don't employ digital pathology, yet......Given how important lighting is in light microscopy, I feel the same thing can be said about digital pathology”.
A few of our participants have extensive digital pathology experience and amongst these colleagues, it was commented that different display luminance preferences have emerged—akin to the variation seen across microscope users (P15). Increasing the luminance of the display was described as helpful for the diagnostic image but after a longer period of reporting becomes too uncomfortable and tiring (P8). Another colleague also commented that mitoses are easier to identify when the display backlight is increased (P5).
Our searches identified work by Tomes and Finlayson (2016) to create a low-cost integrating light sphere with a 3D printer for measurement of photoluminescence quantum yield which was subsequently validated by da Cruz Junior and Bachmann (2021).30,31 We decided to use a similar approach to develop an integrating light sphere-like adaptation for our LXCan light meter. Key features of the design were portability (to allow use in multiple consultant offices), adaptability (to allow use with the range of microscopes in our department) and compatibility with our existing light meter. Using the principles of an ILS our model was designed and tested.
A subset of the main cohort was invited to take part in a practical measurement of their light preferences at the microscope and digital displays. This cohort comprised 40 consultants at a large tertiary teaching hospital (Leeds Teaching Hospitals NHS Trust), which underwent a full workflow digitization in 2018. All consultants in this center have high specification medical grade displays (Jusha C620L) selected for digital reporting as part of the digital deployment programme which uses a Sectra PACS slide viewing software and was deployed according to manufacturer recommendations. The consultant microscopes are of varying make, model and age. Within the department, there is mixed digital pathology experience and competence, ranging from minimal to full time use for primary reporting and other functions.
Light microscopes are illuminated using a complex sequence of lenses and diaphragms in a process called Köhler illumination which achieves uniform illumination of the sample and provides high sample contrast. This is achieved by ensuring the image of the light source is perfectly defocused in the sample plane and conjugate image planes, i.e., the illuminating rays pass parallel through the sample. The amount of light entering the sample can be controlled by the condenser diaphragm or by reducing power to the light source.
Frequency of light adjustments on microscope and display reported by survey participants. Survey participants who indicated they adjusted the light of their equipment during reporting were asked to indicate the frequency of these adjustments on the following scale: 1=never, 5=half of reporting sessions, 10=every case. Microscope users (n=52) and digital reporters (n=7).
There is a rapid increase in the clinical use of digital pathology internationally. The promise of improved workflows, better connectivity between pathologists and providing services to remote locations are the driving force for this change and digital pathology is frequently cited as part of the solution to address an international shortage in the pathology workforce.1 The FDA granted licensing for the first clinical digital pathology system in 2017, which provided regulatory support and thus facilitated policy makers through to pathology departments in the push to “go digital”.2
Optimal lighting levelon microscope
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Increases or decreases thelightintensity microscope
Our survey was conducted by a large sample (64 pathologists across 6 NHS trusts) with a good response rate (59%) and respondents across the full age range, who represent a mix of experience (trainees and consultants) and working hours. Responses in relation to microscope light use habits and opinions should generalize well. The variation in digital pathology experience of this cohort, ranging from no experience to confident primary reporting, means display light use habits and opinions may be less generalizable. We do not have data relating to number of years pathology experience but are aware that in other aspects of reporting it has been shown to impact reporting habits, such as scanning and zooming, so it would be a useful consideration for future studies.20
We conducted an online survey across six NHS hospitals, totalling 108 practicing pathologists, to capture brightness adjustment habits on both microscopes and displays.
We conducted a survey of six pathology departments in the UK to understand perspectives on, and variation of, light use at both the display and microscope. We then designed a practical experiment to capture the working light preferences of pathologists at both the microscope and display to test our hypothesis that microscope light preferences would correlate with display preferences and could be used as a predictor for display setup. This work did not evaluate diagnostic performance or confidence when viewing images.
Free-text comments also suggest that the infrequency of display adjustment seen in this cohort may represent several different issues. Some respondents do not use digital pathology so have no practical need to. Some digital pathology users “have never thought to do so”, assuming “once the display is calibrated it should be suitable for displaying all digital images”. Whilst other users “have never actually figured out how to turn the brightness down! By the end of the day, my eyes tend to get quite fatigued” or have concerns about how the changing the settings would affect diagnostic capability “I am aware that there is some research into potentially missing things on dimmer settings so would be cautious to change without approval/advice”.
Using the scripted protocol, pathologists were asked to “Please make any adjustments to the room, your equipment or yourself that you would ordinarily make before reporting. This may include amendments to the light, the position of your equipment or furniture or removing or adding eyewear”. Ambient lighting and equipment position was recorded at this point.
Our results confirm the anecdotally observed difference in light use between pathologists at the microscope. Analyses of multiple aspects of pathologist reporting activities have been conducted previously but this is the first attempt to describe light use as far as we are aware.18, 19, 20 The accompanying survey provides richer context by capturing the wide variation in frequency of adjustments and the multifactorial reasons for doing so, as well as providing opportunity to gather pathologist opinions on the importance of light adjustments for their work. Of note, light adjustment at the microscope provides pathologists with a compensatory mechanism to adjust for laboratory quality issues, such as thick sections, which cannot be achieved by increasing display backlight. Such slide quality issues would be better addressed by quality control processes within the laboratory.
An integrating light sphere (ILS) is a spherical cavity coated in a highly reflective material which allows incoming light to undergo multiple reflections so that the intensity of the light becomes uniform. Some part of this reflected light can then be measured by a detector placed at a port within the sphere. Integrating light spheres are used in a variety of settings and can measure many different light sources, however from a review of available products, there was no existing model which would be practical or affordable for this project.
The pre-experiment display luminance was recorded on a demonstration pathology image (whole-slide image of liver parenchyma scanned at 40× magnification (0.26 μm per pixel) on an Aperio GT450 scanner) which participants were asked to center on the pre-defined region of the image. The backlight was then reduced to its minimum by the experiment controller. As the light was then gradually increased, participants were asked to state when the light level had reached their preference for viewing the image. This process was then repeated three times with a test slide (a whole-slide image of breast tissue containing invasive carcinoma).
An online survey was designed to capture the light use habits and preferences of pathologists across the West Yorkshire Association of Acute Trusts Region in the UK. This region includes 108 pathology consultants and trainees, working across six different NHS trusts. At the time of writing, the pathologists in these trusts were in the middle of a region-wide deployment of digital pathology and have differing experiences of digital pathology. This ranges from departments with limited or no experience of digital pathology to a department with a fully enabled digital workflow.
At the end of the experiment, participants were invited to comment on any thoughts about light use on their equipment generally or thoughts about the experiment. Comments from during the experiment were also noted.
Experience suggests pathologists have personal preferences for brightness when using a conventional microscope which we hypothesized could be used as a predictor for display setup.
As expected, there was quite variable usage of digital pathology. Time spent viewing digital images ranged from 0 to 25 hr and viewing slides on a microscope ranged from 1 to 50 hr with several pathologists using a combination of modalities (Fig. 3). Twenty-three percent describe no use of digital pathology at all. While for 15% primary reporting was their predominant usage, the most prevalent use of digital pathology was for teaching and training (45%), with smaller numbers using for multidisciplinary team meetings (12.5%) and secondary opinions (3.1%).
Requirement for ethical oversight in this study was waived on review by Leeds Teaching Hospitals NHS Trust Research and Innovation department. Subjects in this study gave informed consent for their participation. Samples of human tissue were used in generating the slides and images used in part of this work. Informed consent was not obtained for this, as these were surplus tissue samples remaining after diagnosis and used as control tissue, they were fully anonymized, and their use without specific consent was approved by a research ethics committee (Leeds West LREC reference 05/01205/270).
There was notable variation in the pre-experiment settings on the displays, ranging from 120 to 345 cd/m2 (0–100 on the monitor backlight scale setting). As part of the deployment, these monitors were installed with a standardized default backlight setting. This indicates that pathologists, or those supporting pathologists with their display setup, have previously adjusted the backlight intensity.
In general, no correlation was seen between microscope and display preference. Two participants had markedly higher display luminance prferences , and this did correlate with the highest microscope light preferences. If excluding these participants as outliers (P6 and P18) there is no statistical correlation (correlation coefficient, r=0.163).
Currently, there is a paucity of guidelines relating to displays used for digital pathology making procurement decisions, and optimal display configuration, challenging.
However, for healthcare services going digital requires a significant initial financial outlay, which was reported to be a key barrier to adoption in a 2018 survey of UK pathology departments.3 Part of this expense includes the procurement of the relevant hardware required for digital pathology workflows and includes the displays on which pathologists will report whole-slide images.4 A vast array of displays are available ranging across medical grade, consumer-off-the-shelf and professional models, with widely varying associated costs.5,6 Navigating the many described specifications of these displays is challenging but key parameters have been proposed to include luminance, contrast, color accuracy, resolution and “just noticeable difference”.6,7 Currently, there is no consistent guidance about the specifications required for these displays as illustrated by Chong et al. where the minimum requirements for a range of national guidelines cover a display size range of 17–27″ and a luminance maximum of 100–300 cd//m2.8 Williams et al. recommended a minimum specification of 24–27″ and 250–350 cd/m2 in guidance for remote reporting on pragmatic grounds.9
Results from the light preference task indicate that pathologist preferences are present. For many of these are consistent within a relatively narrow range. Whilst preference ranges are generally wider for the display, our results indicate that a “one size fits all” approach to display setup will not suit all pathologists.
This section collects any data citations, data availability statements, or supplementary materials included in this article.
For departments looking at procurement of digital displays—it's useful to note that average preferences of all pathologists in this study were <500 cd/m2 and that 85% preferred display luminance of 300 cd/m2 or less. This was surprising given previous work in this department where a range of displays were evaluated by pathologists for digital pathology viewing and the highest luminance monitor (up 2100 cd/m2) was preferred.5 However, experience with digital pathology in the department has matured since this time, when a digital clinical workflow was not yet established. We suspect the difference of participants between the two studies as well as increased personal experience and appreciation of visual fatigue in our cohort may account for the lower luminance preferences in our study. However, there are other differences in the image chain to consider as part of the transition to a digital clinical workflow, such as image management system.
All of the respondents thought it was important or very important to be able to adjust the light on the microscope. Despite minimal reported adjustment of displays in this cohort, 77% felt it was important or very important to be able to do so, with the remaining 23% saying they were uncertain.
These differences were further elaborated on in free-text comments, with selected examples provided in Table 1. At the microscope, light adjustment is used as a compensatory factor for laboratory factors, such as thick sections, however “A brighter display doesn't particularly change the ability to report e.g. thick or overstained sections”.




 Ms.Cici
Ms.Cici 
 8618319014500
8618319014500