Speed Limit 50 mph sign, MUTCD R2-150, Reflective ... - 50 sign
I also tested it out every week for 3 months and it lasted through the end of the second month. Highly recommend following the instructions and charging a few hours every month.
Set limits demonstrating your intent and desire to be of help but not to be abused by the patient. If the patient is causing the clinician to feel uncomfortable, this must be acknowledged. Often telling the patient that his behavior is frightening or provocative is helpful if it is matched with an empathic statement that the desire to help can be interrupted or even derailed if the clinician feels angry, fearful, etc.
The only true measure of the stopping power of a stun gun is microcoulombs (μC). A microcoulomb is a measure of electrical quantity; the millionth part of one coulomb. The higher the μC value, the more it hurts
I may earn a small part of the sale from links to any products or services on this site. You do not pay anything extra and your purchase helps support my work in bringing you more awesome gun and gear articles.
Plus, since this model uses a rechargeable battery, it needs to be charged for an hour or two each month, even if it hasn’t been used.
We have a full review that goes into all the details and accessories (extra cartridges and holsters). But the Taser Pulse is our pick if you’re going to be carrying a Taser as a civilian.
Agitation is an acute behavioral emergency requiring immediate intervention. Traditional methods of treating agitated patients, ie, routine restraints and involuntary medication, have been replaced with a much greater emphasis on a noncoercive approach. Experienced practitioners have found that if such interventions are undertaken with genuine commitment, successful outcomes can occur far more often than previously thought possible. In the new paradigm, a 3-step approach is used. First, the patient is verbally engaged; then a collaborative relationship is established; and, finally, the patient is verbally de-escalated out of the agitated state. Verbal de-escalation is usually the key to engaging the patient and helping him become an active partner in his evaluation and treatment; although, we also recognize that in some cases nonverbal approaches, such as voluntary medication and environment planning, are also important. When working with an agitated patient, there are 4 main objectives: (1) ensure the safety of the patient, staff, and others in the area; (2) help the patient manage his emotions and distress and maintain or regain control of his behavior; (3) avoid the use of restraint when at all possible; and (4) avoid coercive interventions that escalate agitation. The authors detail the proper foundations for appropriate training for de-escalation and provide intervention guidelines, using the “10 domains of de-escalation.”
Multiple people verbally interacting can confuse the patient and result in further escalation. While the designated person is working with the patient, another team member should alert staff to the encounter, while removing innocent bystanders.
Where to buy a Taser gun
That said, that also means that a stun gun doesn’t offer the same level of incapacitation as a firearm…so you’ll need to weigh these implications against each other when deciding whether a stun gun or firearm is better for you.
Written by American gun enthusiasts, competitive shooters, former military/law enforcement personnel, and trained journalists, we use our extensive skill sets and knowledge to bring a well-rounded, researched approach to our content.
I always take the Voltage number with a grain of salt since there’s an asterisk on every stun gun saying something along the lines of it will vary, etc.
According to Lazare and Levy,28 humiliation is an aggressive act where a person has threatened another person's integrity and very self. In some cases, humiliation itself can be traumatic. Therefore, do not challenge the patient, insult him, or do anything else that can be perceived as humiliating.
I’ve tested the stun capability every week for 3 months and it’s still going strong. However you should probably charge it a few hours every month. It has a rechargeable battery with an accompanying separate cord.
Charging is done via a cord attached to the bottom of the unit. I’ve tried it every week for 3 weeks and it’s still going strong. But go with the instructions and charge a few hours every month especially if you’re using it as a flashlight.
Great to give you a little distance…I’d say I’m comfortable shooting it up to 15 feet. Much better than the literal contact distance needed with a traditional stun gun.
Hello, Eric. Good article. Over twenty years ago I bought two of the original Taser Bolt models for my wife daughter. Both still function, but parts are no longer available. I will replace both of those with the newer Taser Bolt 2. Why not the Taser Pulse for the replacements? Well, if they are going to carry what looks like a firearm, then they’ll carry their Glocks. If somewhere that’s not possible, then the outward appearance of the Bolt / Bolt 2 is, in my mind, less likely to cause them to be immediately shot by an antagonist or mistaken for bad guys by Police and shot ’friendly’. Both the Pulse and Bolt 2 are equally capable. To each their own, but the best choice is avoid trouble, or de-escalate, and a gun looking object is most likely to escalate. My two cents…
Modern clinical thinking endorses less coercive interventions, in which the patient becomes a collaborative partner with staff members in managing behavior. These approaches may result in many benefits over traditional procedures. Patients spiraling into agitation can be calmed without forced medication or restraint; most importantly, such benign treatment can empower the patient to stay in control while building trust with caregivers. This may help patients to confidently seek help earlier in the future, and avoid subsequent episodes of agitation altogether.
This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/licenses/by-nc/4.0/.
Natural skill at verbal de-escalation exists on a continuum. However, almost anyone can learn de-escalation techniques and use them successfully if he is well trained and adopts a certain skill set. The most essential skill is a good attitude, starting with positive regard for the patient and the capacity for empathy. Staff should be able to recognize that the patient is doing the best he can under the circumstances, ie, the patient is experiencing difficulty in conforming to what is expected of him. Clinicians in emergency settings also will need to be skilled at recognizing that the inability to conform is due to either cognitive impairment—for example, delirium, psychosis, intoxication, and intellectual disability—or the patient's lack of the skills needed to effectively get his needs met, eg, personality disorder.
We pride ourselves on hands-on testing and real-world experience with all products we recommend. Further, we believe in objectivity and approaching all articles without bias – our few advertisers never influence our reviews or recommendations. We believe in giving our readers a comprehensive understanding of how and why a product is great – or isn’t. And if it’s good enough for us to use ourselves and recommend to loved ones.
A downside is that once you shoot and don’t hit…you’re not really going to be reloading with speed. Sure there’s cartridges but removing and putting a new one in is tough on the clock.
If you know that you would personally have a hard time delivering a fatal blow to an attacker, a stun gun is better than a gun you won’t be able to bring yourself to use.
Some behaviors, eg, punching a wall or even breaking a chair, may not automatically indicate the need for seclusion or restraint, and the patient can continue to be de-escalated with some increase in limit setting and consequences. Reassure the patient that you want to help him regain control and establish acceptable behavior.
A stun gun is a smaller device that delivers the shock through direct contact with the assailant via electrodes on the device.
You’ll generally need to hold the stun gun against your attacker for three to five seconds. A large or particularly determined attacker may need a few additional seconds.
Make sure you’ll actually be able to quickly fire off the stun gun when you need to. If you need to push a lever, slide a switch, and then press a button — will you actually be able to do that under duress?
How does the light compare as a real flashlight? You can obviously find better dedicated lights out there (see our Best Tactical Lights) but it’s still decent.
These options have the added advantage of surprising an attacker — especially if you’re a man pulling out what appears to be lipstick.
This involves persistently repeating your message to the patient until it is heard. Since the agitated patient is often limited in his ability to process information, repetition is essential whenever you make requests of the patient, set limits, offer choices, or propose alternatives. This repetition is combined with other assertiveness skills that involve listening to the patient and agreeing with his position whenever possible.19
You obviously want to avoid hitting yourself, but you won’t be hurt if the attacker is touching you when you hit them with the stun gun, so take any opportunity you have.
Traditional methods of treating agitated patients, ie, routine restraints and involuntary medication, have been replaced with a much greater emphasis on a noncoercive approach. Experienced practitioners have found that if such interventions are undertaken with genuine commitment, successful outcomes can occur far more often than previously thought possible. In the new paradigm, a 3-step approach is used. First, the patient is verbally engaged; then a collaborative relationship is established; and, finally, the patient is verbally de-escalated out of the agitated state. In some ways, this is a return to Lazare's methods published in an article written more than 35 years ago.1
You have to keep in mind that stun guns are WORTHLESS. There is a reason they don't issue these to cops. They flat out don't work (other than pissing people off). A taser actually works the better part of 95 percent of the time. (and that 5 per cent of the time is either those situations where non-lethal force is not appropriate to the situation or else those situations in which you're dealing with someone that has unusual physical attributes / training which tend to make electroshock weapons ineffective.
Greetings, Most of the time the Advertisers Utilize Gigantic Voltage Claims to promote their products. They want you to consider all these massive voltage claims as making their Stun Guns The Best. It would take much more space to present the statistics pertaining to differences in voltage/amperage in batteries, For example 9 volt rechargeable batteries don't produce 9 volts. Some batteries have built-in regulators to the point that they won't even work/function in a stun gun. They are now at claiming some Stun Guns to be producing voltage in the Billions, doesn't that seem very impressive??? The Voltage is a carrier of sorts but not the entity that disrupts the body functions of your Attacker!!! The amperage conducted into the Attacker is your defensive power. It can Kill a human being if too high. So it is regulated by law in this Country to a safe balance between disabling & killing. Of Course it can affect/effect different people in extremely different ways depending on a huge list of factors. Drugs, Clothing, Size, Physical Makeup, Age, Etc., Etc., Etc. The main point I want to Impact, Present, Pound into your Mnd is the requirements of success in saving your own Life are much more than placing your Stun Gun against your attacker while pushing the trigger & Magically Saving Yourself. Some of the Movie Presentations are more than ridiculous. As just presented, it may take "5 Seconds To Longer" to accomplish your Survival/Escape. Stop for a minute, find a clock/watch second hand somewhere and examine what a five second time span really is. "one thousand one, one thousand two, one thousand three, one thousand four, one thousand five" Are you getting the picture? It will feel like a lifetime. It Will Determine Your Lifetime. This conflict will require you to focus "Your Everything You Have" into holding your stun gun in "Continuous Contact" in a generally defined area on Your Assailant . Remember their body is not going to be stationary while you attempt to accomplish this mandatory requirement. You are probably going to have to lock onto them, possibly even going to the ground with them. If you are successful in this very serious challenge, you will have plenty of time to escape this horrible, terrifying Assault on Your Person. If this sounds frightening to you, then think of the other outcomes that are very possible. Don't just buy a Stun Gun, Demand, Search, Question, until you feel qualified to use it. "YES, Stun Guns Can Save Your Life But Not By Themselves, So To Say/So To Speak" They are just a Tool, a Defencive Weapon. Their success is directly Dependent On YOU. YOU NEED TO WIN, YOUR LIFE COULD DEPEND ON IT!!! YOUR FAMILY NEEDS YOU, THEY NEED YOU TO SURVIVE & COME HOME!!! If you are still reading, I Pray this will be of assistance because there is so much more. Blessings Of Health & Happiness Be Upon All Your Families, Be Safe, Be Well
Most older people do not have the option to take up karate or work on there ground and pound. That's why they made Smith and Wesson. However, maybe there are these people that do not feel comfortable carrying a gun and there more concerned with living with themselves after killing someone. Whatever narrative or doctrine you represent in regards to your self protection, its yours. The stun gun can be a great option and it has it place. Just saying.
TASER self defense
Note, the battery comes completely drained and you need to charge a full 8 hours or else it won’t work properly. It says it in the instructions and they were right!
Though the stun sound and distance is less than our other favorites…you give up a little for the size and concealability.
Agitation exists on a continuum, eg, from anxiety to high anxiety, to agitation, to aggression.6 The agitated patient may be unable to engage in any conversation, and may be on the edge of new or repeated violence, requiring vastly different management than a person who may be willing and able to engage. The Project BETA (Best practices in Evaluation and Treatment of Agitation) guidelines7 discussed in this section will help shape a practical, noncoercive approach to de-escalating agitated patients regardless of etiology or capacity to engage in a therapeutic relationship.

Taser gun under 100
The whole point of a stun gun is to deliver a powerful shock, but what prevents an accidental zap? Some stun guns also have features that render them unusable if it’s taken from you.
Stun guns use either rechargeable lithium-ion batteries or replaceable batteries. Replaceable batteries mean you never have to wait for the stun gun to charge, but built-in rechargeable batteries typically have greater battery life and are capable of delivering a greater shock.
For the patient who has nothing left but to fight or take flight, offering a choice can be a powerful tool. Choice is the only source of empowerment for a patient who believes physical violence is a necessary response. In order to stop a spiraling aggression from turning into an assault, be assertive and quickly propose alternatives to violence. While offering choices, also offer things that will be perceived as acts of kindness, such as blankets, magazines, and access to a phone. Food and something to drink may be a choice the patient is willing to accept that will stall aggressive behaviors. Be mindful that these choices must be realistic. Never deceive a patient by promising something that cannot be provided for him. For example, a patient should not be promised a chance to smoke when the hospital has a no-smoking policy.
Instrumental aggression is used by those who have found they can get what they want by violence or threats of violence. This aggression is not driven by emotion and can be handled by using unspecified counter offers to the aggressor's threat. If a patient threatens to hurt someone if he doesn't get a cigarette, a counter offer might be, “I don't think that's a good idea.” The patient's next response may be, “What do you mean?” A counter offer would be, “Let's not find out.”
Finally, when verbal attempts to de-escalate fail, more coercive measures such as restraints or injectable medication may be necessary to ensure safety but always as a last resort.
Miller's law states, “To understand what another person is saying, you must assume that it is true and try to imagine what it could be true of.”25 If you follow this law, you will be trying to understand. If you are truly trying to imagine how it could be true, you will be less judgmental, and the patient will sense that you are interested in what he is saying and this will significantly improve your relationship with the patient. For example, if the patient's agitation is driven by the delusion that someone is following him and intends to cause him harm, you can imagine how this is true from the patient's standpoint and engage the patient in conversation as to why this is happening to him and who would want to harm him. This will convey your interest and will result in the patient engaging in conversation about that which is driving his agitation. By engaging in conversation, the patient will begin to see that you care, which in turn, fosters de-escalation.
And did a function check every week to make sure each one could carry enough charge. Each tested unit has quick videos to showcase the *cackle* of electricity.
The second form of irritable aggression occurs in persons who are chronically angry at the world and are looking for an excuse to “go off.” They give no reason for their anger. They want to release the constant pressure resulting from their world view. They make unrealistic and erratic demands and use these as an excuse to attack when their demands are not met. They get enjoyment out of creating fear and confusion and may make feigned attacks to intimidate those who are working with them. Do not react in a startled or defensive way. These patients are looking for an emotional response from anyone who is an audience. Don't give them one and remove all other patients, unnecessary staff members, and bystanders from the area. Use emotionless responses. De-escalation involves giving the patient choices other than violence to get what he wants. As he makes erratic demands, use the broken record to return to the options you can offer. Let him know you will work with him but only when he is willing to be cooperative. Set firm limits to protect staff and other patients and intervene with restraint if the limit is violated. Unfortunately, many of these patients will test the limit by doing just what you have asked them not to do and end up in restraints.
General principles of verbal de-escalation can be found in specific psychotherapies, linguistic science, law enforcement, martial arts, and the nursing profession. Clinicians who work with agitated patients on a daily basis have perfected skills that frequently are in line with principles found in these resources. However, a review of the literature indicates that scientific studies and medical writings on verbal de-escalation are few and lack descriptions of specific techniques and efficacy.
Start by explaining why the intervention was necessary. Let the patient explain events from his perspective. Explore alternatives for managing aggression if the patient were to get agitated again. Teach the patient how to request a time out and how to appropriately express his anger. Explain how medications can help prevent acts of violence and get the patient's feedback on whether his concerns have been addressed. Finally, debrief the patient's family who witnessed the incident.
If you live in or are visiting one of these places, a stun gun is, again, far better than nothing. And if you have to wait to finish a course or face any other delay, you may want to carry a stun gun in the meantime.
Taser gun buy online
Another step is one just short of involuntary medication. “Mr Smith, you're experiencing a psychiatric emergency. I'm going to order you some emergency medicine.” This strategy is authoritative, as in being knowledgeable and self-assured, possessing expertise, having the ability to explain one's thinking, and being persuasive. Giving the patient a choice in either oral or parenteral administration can help give the patient some control. He may willingly take medication if the means of administration is a choice, even if the administration of medication itself is not a choice. Appealing to the patient's desire to stay in control and the clinician's mandate to keep everyone safe, one might say to the patient: “I can't let any harm come to you or anyone else” or “I need to protect you from hurting someone, so I would like for you to take some medication to help you stay in control.” The clinician then says to the patient as many times as necessary, “Would you like to take medication by mouth or by a shot?” Emphasizing the protection aspect is very important and can be effective in empowering the patient to stay in control. “I feel medications can help, would you like a pill you can swallow, a pill that will melt in your mouth, or a liquid? If you agree to take a pill by mouth you can avoid taking a shot.” Even when there is no choice but to give an injection, the clinician can give a choice as to which drug is to be used, emphasizing that one has a more beneficial side-effect profile.
Regardless of underlying etiology, agitation is an acute emergency and “requires immediate intervention to control symptoms and decrease the risk of injury” to the patient or others.11 While voluntary medication and environment planning are also important, verbal de-escalation and nonverbal communication are usually key to engaging the patient and helping him become an active partner in de-escalation.
The use of objective scales to measure agitation can help mitigate defensive behaviors on the part of staff that might result in their avoiding or “ignoring” early signs of agitation. One such scale that is quite simple and easy to implement is the Behavioural Activity Rating Scale (BARS; Table 1).21
If you can’t afford a handgun at the moment, but still want to carry something to protect yourself, a stun gun is far better than nothing — and it can still get the job done.
The Xtreme Sanctuary also comes with an insanely loud alarm activated by flipping the slide button all the way up…something that’s missing on the Vipertek. It will turn heads and hurts my ears even for a few seconds when I activate it indoors.
On top of that, tasers can be pricey to purchase and maintain, and some models have a tendency to be bulky and difficult to conceal.
Since 2016, the Pew Pew Tactical team has been dedicated to providing expert reviews and in-depth testing of guns and gear. All while keeping in mind that guns are fun and that readers come first.
So I have had a stun gun for the house as part of self defense and home defense options should access to lock box pistol be too time consuming. I find that the light is great, but design flaw has it go off when switched to zap; that light as a blinding tool should remain on right up to body contact. As a tool in the toolbox its great because sometimes one has to create space and time to "earn your draw," just as good hand to hand and knife courses teach you.
Examples of wants include succorance, the wish to ventilate to an empathic listener, a request for medication, some administrative intervention, such as a letter to an employer, or intervening with a difficult spouse or parent. Whether or not the request can be granted, all patients need to be asked what their request is.1 A statement like, “I really need to know what you expected when you came here,” is essential, as is the caveat “Even if I can't provide it, I would like to know so we can work on it.”
Stun guns are less regulated than firearms, but they aren’t legal in all places. Be sure to check your local laws before buying one to make sure you won’t be in legal trouble if you ever have to use your stun gun.
So if you’re looking for a small stun gun…you can’t go wrong with the Lifeguard. And don’t worry it comes in pink AND black.
Once the patient is calm, the clinician can acknowledge and work with the patient on a deeper level, help put the patient's concerns into perspective, and assist him in problem solving his initial precipitating situation. Since prevention of agitation is the best way to treat it, planning with the patient is best: “What works when you are very upset as you were today? What can we/you do in the future to help you stay in control?”
To use the stun gun, press the trigger and hold the probes firmly against the attacker, ideally aiming for the torso, particularly the neck, shoulder, underarm, groin, and abdomen between the hip and ribs. If you can’t hit the torso, hit any part of the attacker that you can reach.
Agitation is a behavioral syndrome that may be connected to different underlying emotions. Associated motor activity is usually repetitive and non–goal directed and may include such behaviors as foot tapping, hand wringing, hair pulling, and fiddling with clothes or other objects. Repetitive thoughts are exhibited by vocalizations such as, “I've got to get out of here. I've got to get out of here.”3 Irritability and heightened responsiveness to stimuli may be present,4 but the association of agitation and aggression has not been clearly established.5
Even the most complicated cases can be managed with a little additional time. Assuming that a single interaction of listening and responding takes less than a minute, then a dozen repetitions of the clinician's message would take 10 minutes at the most. De-escalation, when effective, can avoid the need for restraint. Taking the time to de-escalate the patient and working with him as he settles down can be much less time-consuming than placing him in restraints, which requires additional resources once he is restrained.
TASER 10
Security and police officers, who work with agitated patients, must accept that a patient's abnormal behavior is a manifestation of mental illness and that de-escalation is the preferred treatment of choice. The Crisis Intervention Team (CIT) model is a police-based, first-responder program that has been implemented nationwide. Persons taken into custody because of suspected mental illness are taken to a psychiatric emergency service or other facility where the person can receive psychiatric evaluation and treatment. CIT officers usually volunteer for these teams so that an officer is not forced into taking on a role that he does not want. Training of officers is provided by mental health professionals, legal experts, and advocates.16,17
have you ever tested a stun gun for 1 million + volts? maximum voltage that can pass between the electrodes is around 30,000 MAX....
When choosing a stun gun, you’ll want to pay particular attention to a few different traits. These are important in more ways than one!
The physical environment is important for the safe management of the agitated patient. Moveable furniture allows for flexible and equal access to exits for both patient and staff. The ability to quickly remove furniture from the area can expedite the creation of a safe environment. Some emergency departments prefer stationary furniture, so that the patient cannot use the objects as weapons, but this may create a false sense of security. There should be adequate exits, and extremes in sound, wall color, and temperature of the environment should be avoided to minimize abrasive sensory stimulation. Be mindful, also, of the potential for an agitated patient's throwing objects that may cause injuries to others. Any objects, such as pens, sharp objects, table lamps, etc that may be used as weapons should be removed or secured. The clinician should closely monitor any objects that cannot be removed.
A stun gun requires you to contact two points to an assailant while typical TASERs shoot out prongs at a distance. However, TASER has recently come out with contact models.
25,000 volts typically will deliver pain to your assailant. However higher voltage in the 50,000 to 100,000 volt range is better especially with clothing covering the skin.
De-escalation frequently takes the form of a verbal loop in which the clinician listens to the patient, finds a way to respond that agrees with or validates the patient's position, and then states what he wants the patient to do, eg, accept medication, sit down, etc. The loop repeats as the clinician listens again to the patient's response.19 The clinician may have to repeat his message a dozen or more times before it is heard by the patient. Yet, beginning residents, and other inexperienced clinicians, tend to give up after a brief attempt to engage the patient, reporting that the patient won't listen or won't cooperate.20
The Vipertek VTS-T03 is a poor choice in my opinion. I can't imagine trying to find and press that tiny stun button under stress, while fending off an attacker. A lot of budget gun seem to do this. Why would you have a button smaller than a pencil eraser, flush with the surface and the same color as the gun? I want a button as big as my thumb that sits an 1/8" proud and in fluorescent orange.
The higher the voltage, the stronger the shock. You want a stun gun that shoots at least one million volts. Stun guns that shoot less are generally sacrificing quality for the price.
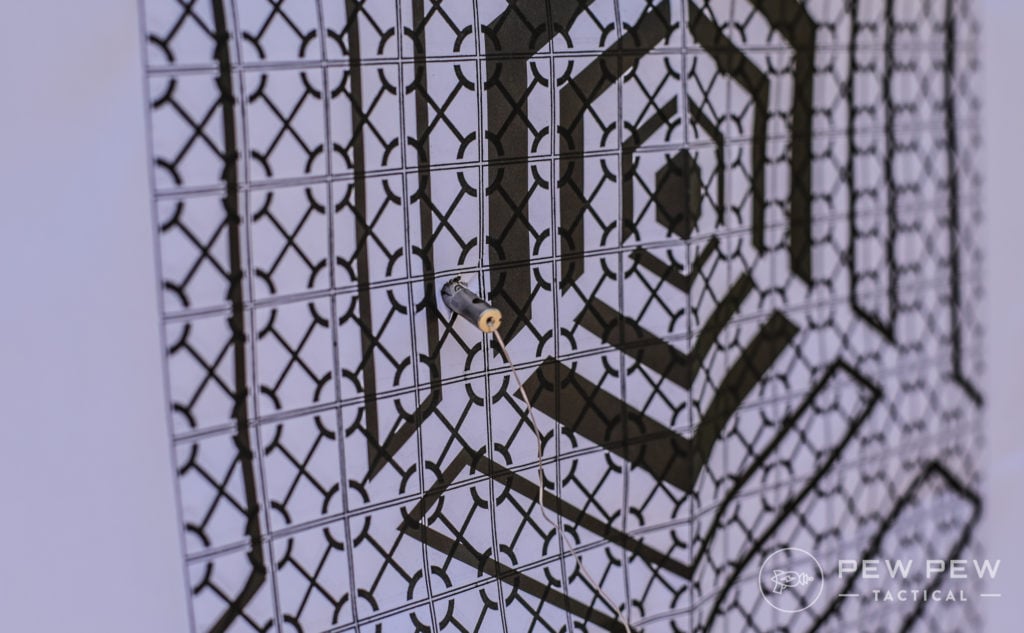
For TASER units we shot them at 15-feet away electrically-wired targets to test listed range, expansion of prongs, and ability to incapacitate.
If the patient does not mention medication and the clinician believes it is indicated, then state clearly to the patient that you think he would benefit from medication. Ask the patient what medication has helped him in the past or state, “I see that you're quite uncomfortable. May I offer you some medication?”
Training in management of the agitated patient decreases the tendency of clinicians to avoid working with these patients. The American Psychiatric Association Task Force on Psychiatric Emergency Services18 has recommended that staff receive annual training on managing behavioral emergencies. This training is analogous to advanced cardiovascular life support training, ie, knowledge about skills can be taught in a classroom or can be learned from a book, but skills come only with practice. De-escalation skills can be learned by role playing and can be practiced in day-by-day encounters with nonagitated patients who are considered to be difficult in the sense of not conforming to what the clinician expects.
Irritable aggression comes in 2 forms. The first is the patient who has had boundaries violated. Someone has cheated him, humiliated him, or otherwise emotionally wounded him. He is angry and trying to put his world back together, ie, he is trying to regain his self-worth and integrity. This patient wants to be heard and have his feelings validated. This type of aggression is identified by the patient's telling you what has made him angry. De-escalation involves setting conditions for the patient to be heard. Fogging and the broken record approach19 are most helpful. A typical scenario is the patient who found out that his girlfriend had cheated on him. His friends kidded him and a fight ensued. He was brought in by police. On arrival the patient is furious. He states that his girlfriend had cheated on him and that the police are treating him unfairly. The initial response is to agree in principle that the patient's anger is justified. This is followed by telling the patient that you want to know more but cannot until he regains control so that “we can talk.” The patient may respond that nobody understands. The response is that he may be right but you would like to try to understand. This loop may need repeated a dozen or more times before the patient complies.
If restraint or force needs to be used, it is important that the staff be debriefed on the actions after the event. Staff should feel free to suggest both what went well during the episode, and what did not, and recommend improvements for the next episode.
Far from an expert. You are dealing with high voltage but low amperage. If, you are in contact with the criminal are you not shocked as well?
Emergency psychiatry is a well-established mental health discipline. However, the number of emergency psychiatrists and the volume of psychiatric crises they see are limited when compared to the number of emergency department physicians evaluating psychiatric emergencies. Interventions must often proceed with the agitated patient with, at best, a tentative diagnosis.
The only true measure of the stopping power of a stun gun is microcoulombs (μC). A microcoulomb is a measure of electrical quantity; the millionth part of one coulomb. The higher the μC value, the more it hurts
A good strategy is to be polite. Tell the patient your title and name. Rapidly diminish the patient's concerns about your role by explaining that you are there to keep him safe and make sure no harm comes to him or anyone else in the emergency setting. If the patient is very agitated, he may need additional reassurance that the clinician wants to help him regain control. Orient the patient as to where he is and what to expect. If the patient's name is unknown, ask for his name. Judgment is required in deciding whether to call the person by his first or last name. Although some prefer calling all patients by their last names, this formality, in some situations, can add to a patient's suspicion and appear patronizing. When in doubt, it is best to ask the patient how he prefers to be addressed; this act communicates that he is important and, from the very beginning of the interaction, that he has some control over the situation.
Taser Amazon
There are patients who cannot be effectively engaged and verbally de-escalated, eg, a delirious patient. However, training should emphasize that a patient may not respond to initial efforts to engage him in de-escalation and that persistence is indicated, especially when the patient is not showing signs of further escalation that is moving toward violence.
It also has two metal strips that go down the sides of the top of the device from the electrodes, preventing the device from being taken away from you.
You ever review just flashlight stun guns with concealed or discreet prongs? Had 2, don't remember which, and they both fell apart. Safety switch on the back made it less available and resulted in me stunning myself a few times leaving the safety off. After that, they all sound shady, but i need a new one. Already had an incident where it would have been nice to have it and probably would have saved us all from a lot of trouble and harm done.
Gentle confrontation may also be useful: “It's important for you to be calm in order for us to be able to talk. How can that be accomplished? Would you be willing to take some medication?”
If the stun gun isn’t easy and comfortable to carry, you’ll probably just leave it at home. A compact model will be easier to carry and conceal, but there are also covert options that look like everyday objects like a cell phone or lipstick.
I'm Eric Hung, the founder of Pew Pew Tactical, and I love guns. For over 10 years I've been soaking up as much information as possible online, in competitions, classes, and from my own testing. Now I hope to bring that info to you! I've written over 250 articles on Pew Pew Tactical that are read by millions a month. I'm also an NRA certified pistol instructor and avid USPSA/3-Gun/NRL22 competitor. Learn more at About Us.
The clinician must convey through verbal acknowledgment, conversation, and body language that he is really paying attention to the patient and what he is saying and feeling. As the listener, you should be able to repeat back to the patient what he has said to his satisfaction. Such clarifying statements as “Tell me if I have this right…” is a useful technique. Again, this does not mean necessarily that you agree with the patient but, rather, that you understand what he is saying.
Activation of the stun button is very similar for both models with a flip switch on the side opposite the slider mode switch. And both models come with side shock plates so baddies can’t grab it away from you.
It charges via a small port and is still holding a charge after 3 months. Although, again, follow instructions and charge it up a few hours each month.
It has the same safety mechanism as the VTS-989, but without the grab protection feature, and also features an LED flashlight.
When approaching the agitated patient, maintain at least 2 arm's lengths of distance between you and the patient. This not only gives the patient the space he needs, but also gives the clinician the space needed to move out of the way if the patient were to kick or otherwise strike out. The clinician may want to give himself more distance in order to feel safe; and, if a patient tells you to get out of the way, do so immediately. Both the patient and the clinician should be able to exit the room without feeling that the other is blocking his way.
All persons who work with agitated patients should receive training in de-escalation techniques. A person, who is appropriate for the job, as discussed earlier, should be the one who works directly with the patient. A psychiatrist, emergency physician, or any other healthcare worker can become proficient at de-escalation, and any of these can engage the patient and perform de-escalation.
For one, tasers are illegal under many state and local laws, and even where they are legal, acquiring one has the added difficulty of a background check.
Fear driven aggression is not self defense. The patient wants to avoid being hurt and may attack to prevent someone from hurting him. Give the fearful patient plenty of space. Do not have a show of force or in any other way intimidate the patient or make him feel threatened, as this will feed into the patient's belief that he is going to be hurt. De-escalation involves matching the patent's pace until he begins to focus on what is being said rather than his fear. If the patient says, “Don't hurt me. Don't hurt me.” Counter with the same pace by saying, “You're safe here. You're safe here.”Try to decrease the pace tohelp the patient calm down.
After any involuntary intervention with an agitated patient, it is the responsibility of the clinician who ordered these interventions to restore the therapeutic relationship to alleviate the traumatic nature of the coercive intervention and to decrease the risk of additional violence.
Your "Best Beginner Handguns" link is broken. It should point to https://www.pewpewtactical.com/best-handgun-beginners-home-defense/
Be optimistic but in a genuine way. Let patients know that things are going to improve and that they will be safe and regain control. Give realistic time frames for solving a problem and agree to help the patient work on the problem. When the patient states, “I want to get out of here,” the clinician can respond, “I want that for you as well; I don't want you to have to stay here any longer than necessary; how can we work together to help you get out of here?”
There is indirect evidence from pharmacologic studies of agitation that verbal techniques can be successful in a substantial percentage of patients. In a recent study, patients were excluded from a clinical trial of droperidol if they were successfully managed with verbal de-escalation; however, the specific verbal de-escalation techniques were not identified or studied.12
A sad person wants something he has given up hope of having. A patient who is fearful wants to avoid being hurt. In a later discussion of aggression, it will be apparent that the aggressive patient has specific wants also, and identifying these wants is important for the management of the patient.
You should choose the one (or ones) that best fits your lifestyle. If you’re looking for a real firearm though, you won’t go wrong choosing from one of our Best Concealed Carry Handguns.
I have the Viper 989 stun gun. I do like to very much however, the case it comes with is useless. It is a cheap lightweight thin material that is so tight, you need two hands to pull out the stun gun. If it is on your belt. You will not be able to get it out fast enough. Why they would make such a good product in the gun but use such cheap non fitting case is beyond me. But unless you are planning to use a tactical holster for e a stun gun, buy another product.
Volts are fine, but the real measure is where it stands on the uC pain scale. A billion volts is great, unless it hits the uC scale at less than 1.0. Where do these hit the scale.
Another great option would be pepper spray and depending on where you live, pepper spray might be legal where a stun gun isn’t — or the other way around.
I believe in Florida you need a concealed carry permit to carry a stun gun or pepper spray. Sense,, that everyone agrees on, simply will not happen.
However the Xtreme Sanctuary’s 150 million volt cackle is ominous sounding and I would definitely not want to get hit by it.
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Most powerful stun gun on Amazon
Finally, each clinician must remember the 4 main reasons for using noncoercive de-escalation. First, when staff members physically intervene to subdue a patient, it tends to reinforce the patient's idea that violence is necessary to resolve conflict. As such, noncoercive de-escalation is a success for the patient and staff, and is in effect a form of treatment. Second, patients who are put in restraints are more likely to be admitted to a psychiatric hospital8 and have longer inpatient lengths of stay.9,10 Third, the Joint Commission and the Centers for Medicare and Medicaid Services consider low restraint rates a key quality indicator, and fourth, staff and patients are less likely to get hurt when physical confrontation is averted.
The bottom line is that good “working conditions” require that both patient and clinician treat each other with respect. Being treated with respect and dignity must go both ways. Violation of a limit must result in a consequence, which (1) is clearly related to the specific behavior; (2) is reasonable; and (3) is presented in a respectful manner.
These objectives may be challenging to pursue in some situations and settings. For example, in an emergency department, both the clinician and patient can slip into irrational thinking or expediency at the price of engaging each other. A clinician who has many patients to see and too little time may prematurely use medication to avoid verbal engagement. However, using medication too quickly may seem dismissive, rejecting, or humiliating to the patient2 and can lead to more agitation and violence.
TASER official is offering Pew Pew Tactical readers 15% off with code PEWPEW. Although at this time The Home Security Superstore’s $70 off brings it down to $329.
When working with an agitated patient, there are 4 main objectives: (1) ensure the safety of the patient, staff, and others in the area; (2) help the patient manage his emotions and distress and maintain or regain control of his behavior; (3) avoid the use of restraint when at all possible; and (4) avoid coercive interventions that escalate agitation.
Another feature is that the charging plug is integrated so no cord to lose. And the size is much smaller than our other favorite on the list.
A clinician cannot be effective if he has too much emotion or is frightened by the patient. Keeping the clinician safe is the first step toward patient safety. Approximately 90% of all emotional information and more than 50% of the total information in spoken English is communicated not by what one says but by body language, especially tone of voice.25 When the clinician approaches the agitated patient, he must monitor his own emotional and physiologic response so as to remain calm and, therefore, be capable of performing verbal de-escalation.26
Our pick if you want something smaller with a built-in charger and also really affordable. However, we still recommend spending a few more bucks for one of our other top picks.
Once you have established a relationship with the patient and determined that he has the capability to stay in control, teach him how to stay in control. Use gentle confrontation with instruction: “I really want you to sit down; when you pace, I feel frightened, and I can't pay full attention to what you are saying. I bet you could help me understand if you were to calmly tell me your concerns.”
The first person to make contact with the patient should be the person designated to de-escalate the patient. If that person is not trained or is otherwise unable to take on this role, another person should be designated immediately.
I agree completely. And just buying one and putting it your purse or pocket is not the answer either. You need to train with it, practice deploying it under stress, be able to manipulate the buttons w/o having to think about it much, ect.
It is critical that the patient be clearly informed about acceptable behaviors. Tell the patient that injury to him or others is unacceptable. If necessary, tell the patient that he may be arrested and prosecuted if he assaults anyone. This should be communicated in a matter-of-fact way and not as a threat.
Stun guns and tasers are some of the most popular forms of self-defense currently available…even more popular than firearms.
The traditional goal of “calming the patient” often has a dominant-submissive connotation, while the contemporary goal of “helping the patient calm himself” is more collaborative. The act of verbally de-escalating a patient is therefore a form of treatment in which the patient is enabled to rapidly develop his own internal locus of control.
Verbal de-escalation techniques have the potential to decrease agitation and reduce the potential for associated violence, in the emergency setting. But while much has been written on the psychopharmacologic approaches to agitated patients, until now there has been relatively little discussion about verbal methods.
A paradigm that can be useful for both psychiatrists and emergency physicians is one in which the clinician uses rapid assessment and decision-making skills in an effort to quickly provide symptom relief. This relief, through verbal de-escalation and/or medication, enhances a positive clinician-patient relationship, decreases the likelihood of restraints, seclusion, and hospital admissions,8 and prevents longer hospitalization, since the use of restraints has been associated with increased length of stay.9,10 After initial stabilization of the patient's agitation, the clinician can work with the patient to establish a final diagnosis.
A Fond memory I have of my ex wife. She didn't like that I CC'd a 1911. She got me one of the old Safariland 90KV shock sticks for my birthday 40 years ago. Not concealable worth a darn. She was enthusiastically demonstrating the features and before I new what happened she had zapped herself on her left thigh and went down like a 130lb bag of wet laundry. I was still laughing as I made myself comfortable on the couch for the next couple of weeks. Honestly? I'd rather carry my 1911.
Be cautious with this kind of weapons. It is a tool and it is not always efficient. Like a pepper spray, it could be a good alternative to lethal force under certain circumstances, and that’s about it. If you have to carry ONE weapon pick a firearm. I carry a taser on duty, and I don’t feel the need to carry any kind of electrical weapon off duty. Firearm, spare mag, knife, and flashlight only. On duty I also like to think my taser does not exist, too many cops become taser dependent and when it is ineffective they don’t know what to do. Again it can be a great tool and deterrent, it is up to you to make the decision, just don’t think it is the best thing ever.
The Xtreme Sanctuary also comes with a much brighter flashlight than the Vipertek. And the flashlight is on when you’re in stun mode. For the Vipertek you can either have the choice of light or stun.
“Free information” comes from trivial things the patient says, his body language, or even past encounters one has had with the patient.19 Free information can help the examiner identify the patient's wants and needs. This rapid connection based on free information allows the clinician to respond empathically and express a desire to help the patient get what he wants, facilitating rapid de-escalation of agitation.
Agitated patients can be provocative and may challenge the authority, competence, or credentials of the clinician. Some patients, in order to deflect their own sense of vulnerability, are exquisitely sensitive in detecting the clinician's vulnerability and focusing on it. To work well with agitated patients, staff members must be able to recognize and control countertransference issues and their own negative reactions. These include the clinician's understanding of his own vulnerabilities, tendencies to retaliate, argue, or otherwise become defensive and “act-in” with the patient. Such behaviors on the part of the clinician only serve to worsen the situation. Clinicians need to also recognize their limits in dealing with an agitated patient, as it can be quite taxing, and sometimes the best intervention is knowing when to seek additional help.
My personal favorite full-size option is the Tiger-USA Xtreme Sanctuary for a great combo of bright light, alarm, and strong stun.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Just received the Extreme Sanctuary Stun Gun. While I am happy with the device, I think another "con" should have been the very short (8.5 inch long) charging cord. Not very convenient unless you're using a countertop outlet.
Looking for something covert? Take a look at the Streetwise Sting Ring that is sort of like a brass knuckle…but with added shock value.
The initial BARS score should be based not only on the patient's presentation, but also on his behavior before arrival at the emergency facility. Any score other than a 4 should trigger an evaluation by a clinician and establish the urgency of that evaluation. Other available scales include the Overt Aggression Scale,22 the Scale for the Assessment of Aggressive and Agitated Behaviors,23 and the Staff Observation Aggression Scale.24
Fogging is an empathic behavior in which one finds something about the patient's position with which he can agree.19 It can be very effective in developing one's relationship with the patient. There are 3 ways to agree with a patient. The first is agreeing with the truth. If the patient is agitated after 3 attempts to draw his blood, one might say, “Yes, she has stuck you 3 times. Do you mind if I try?” The second is agreeing in principle. For the agitated patient who is complaining that he has been disrespected by the police, you don't have to agree that he is correct but you can agree with him in principle by saying, “I believe everyone should be treated respectfully.” The third is to agree with the odds. If the patient is agitated because of the wait to see the doctor and states that anyone would be upset, an appropriate response would be, “There probably are other patients who would be upset also.” Using these techniques, it is usually easy to find a way of agreeing, and one should agree with the patient as much as possible. Clinicians may find themselves in a position where they are being asked to agree with an obvious delusion or something else the clinician can obviously have no knowledge of. In this situation, acknowledge that you have never experienced what the patient is experiencing but that you believe that he is having that experience. However, if there is no way to honestly agree with the patient, agree to disagree.
Clinicians who work in acute care settings must be good multitaskers and tolerate rapidly changing patient priorities. In this environment, tolerating and even enjoying dealing with agitated patients takes a certain temperament, and all clinicians are encouraged to assess their temperament for this work.
3. Sabre S-1005 Dual Stun Gun - price @ $60, not $17 when I looked and no mention in your article or on the Amazon page about how many volts.
Stun gun vs Taser
It’s incredibly powerful with a voltage of 300 million, making it the strongest stun gun on this list. However I’m meh about the ratings and it sounds like the 150 million one.
Working with an agitated patient is a team effort and there must be an adequate number of people to provide for verbal de-escalation, offer the possibility of voluntary medication, and maintain safety if the patient's agitation escalates to violence. There is also a benefit in having enough people to provide a nonverbal communication to the patient that violence on the part of the patient will not be acceptable behavior. In a busy emergency service, the de-escalation team should consist of 4 to 6 team members made up of nurses, clinicians, technicians, and police and security officers, if available.
When medications are indicated, offer choices to the patient. Timing is essential. Do not rush to give medication but, at the same time, do not delay medication when needed. Using increasing strategies of persuasion is a sound technique (Table 3). For example, the first step is not to mention medication at all but to ask the patient what he needs, what works. Try to get the request for medication to come from the patient himself, or perhaps the patient has a better idea.
I have two charge up stun guns that loose their charge quickly. Should I ever need to use them I can be sure they will not work. I want a battery powered stun gun. Which of your stun guns operate with a battery?
A stun gun, on the other hand, is much more affordable, is less legally regulated, and is more compact and easier to conceal, all while delivering the same strength of shock as a taser.
The following guidelines were therefore developed by the consensus of the authors and a review of the limited available literature on verbal de-escalation.13–15
A high percentage of patients have a past history of trauma, and the emergency experience has the potential for repeating the traumatic experience when specific aspects of personal space are ignored. A person who lives on the street may be very sensitive about protecting his belongings. Those who have been sexually abused may be apprehensive about being unclothed, which can increase their sense of vulnerability and cause humiliation.
We’ve built dozens of AR’s and we’ll cover all the best AR-15 upgrades such as handguards, triggers, BCGs, gas blocks, and more.
Although it doesn’t stand up to the new favorite Tiger-USA…the Vipertek is still a good option if you want quick Prime shipping from Amazon.
The goal of medicating the agitated patient is not to sedate but to calm him. As Allen and colleagues11 point out, a calm, conscious patient is one who can participate in his own care and work with the crisis clinician toward an appropriate treatment disposition, which is of benefit to the patient and also to the staff. It can decrease length of stay and make the emergency department experience a positive one.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Now let’s hear from you guys! Do you ever carry a stun gun? Which one? Why a stun gun instead of a firearm or pepper spray?
The amount of time permitted for verbal de-escalation may vary depending on the setting and other constraints. However, it is the consensus of Project BETA De-escalation Workgroup members that verbal de-escalation frequently can be successful in less than 5 minutes. Its potential advantages in safety, outcome, and patient satisfaction indicate it should be attempted in the vast majority of agitation situations, even in very busy emergency settings.
As previously noted the extent of aggression associated with agitation has not been clearly established.5 However, some agitated patients are aggressive and the approach to the patient depends upon the type of aggression. Moyer29 has defined several types of aggression, some of which are commonly seen in the emergency setting. Types of aggression also have been identified in the setting of a correctional facility30 and by martial arts instructors.31 These identified types can be placed in Moyer's classification and are important because principles of management have been developed for each of the different types of aggression. Some of the management techniques used in correctional facilities and taught in the martial arts are not recommended for use in the healthcare setting. However, the principles allow us to develop techniques appropriate to the healthcare setting and are discussed here. It will be apparent that there is always something the patient wants. As discussed earlier, identifying the patient's wants is important and, in this case, determines how the patient is managed.

Since agitated patients may be impaired in their ability to process verbal information, use short sentences and a simple vocabulary. More complex verbalizations can increase confusion and can lead to escalation. Give the patient time to process what has been said to him and to respond before providing additional information.
The clinician must demonstrate by body language that he will not harm the patient, that he wants to listen, and that he wants everyone to be safe. Hands should be visible and not clenched. Avoid concealed hands, which imply a concealed weapon.20 Knees should be slightly bent. The clinician should avoid directly facing the agitated patient and should stand at an angle to the patient so as not to appear confrontational. A calm demeanor and facial expression are important. Excessive, direct eye contact, especially staring, can be interpreted as an aggressive act. Closed body language, such as arm folding or turning away, can communicate lack of interest. It is most important that the clinician's body language be congruent with what he is saying. If not, the patient will sense that the clinician is insincere or even “faking it” and may become more agitated and angry. It is also important to monitor closely that other patients or individuals do not provoke the patient further.




 Ms.Cici
Ms.Cici 
 8618319014500
8618319014500